Table of Contents
Page created on April 28, 2021. Last updated on April 19, 2022 at 12:55
Definition and epidemiology
Chronic obstructive pulmonary disease (COPD) is characterised by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities. It’s common, preventable, and treatable. It is defined as a post-bronchodilator FEV1/FVC ratio of < 0,70.
It affects 11,7% of the world and it’s the third leading cause of death worldwide. Prevalence is expected to rise, and it’s expected to be the leading cause of death in 15 years.
COPD has two phenotypes, chronic bronchitis and emphysema.
Etiology
- Smoking (most important factor)
- Air pollution
- Occupational dusts and chemicals
- Frequent lower respiratory tract infections during childhood
- Alpha-1-antitrypsin deficiency
Pathomechanism
The following factors are involved in the pathomechanism:
- Airway wall inflammation
- Fibrosis
- Smooth muscle hypertrophy
- Goblet cell metaplasia
- Destruction of the alveolar walls
- Mucus hyperproduction
Chronic bronchitis is characterised by narrowing of the airway lumen, mucus hypersecretion and inflammation. Emphysema is characterised by loss of elastic recoil, and alveolar destruction.
Classification
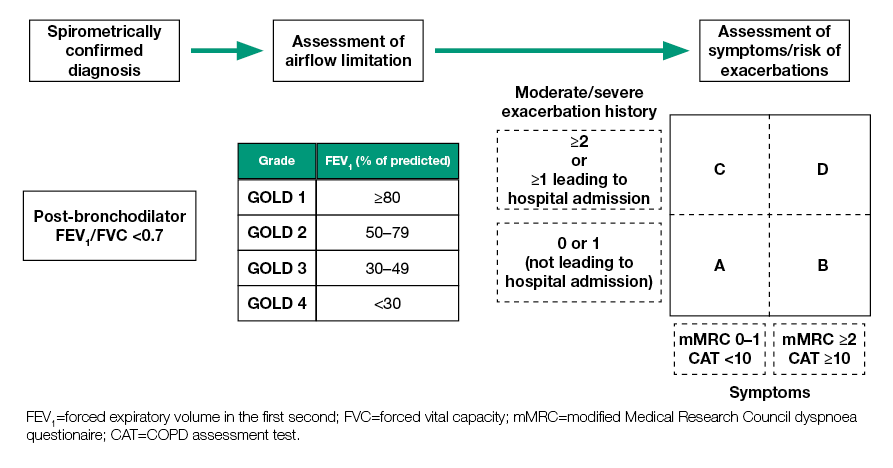
The mMRC scale grades COPD based on the severity of dyspnoea, from 0 (dyspnoea only on exercise) to 4 (too breathless to leave the house, or dyspnoea when doing nothing).
The CAT (COPD assessment test) score grades COPD based on the severity of all symptoms as well as the life quality. There are 8 descriptions which are graded from 0 – 5 based on how much the patient agrees with the description. A total CAT score of > 10 is considered to equal “severe symptoms”.
The mMRC grade and the CAT are used to classify the COPD patient according to the GOLD classification. The patient is given a GOLD number according to their FEV1, and a GOLD letter according to the mMRC, CAT, and number of exacerbations. GOLD 1A is the least severe overall, while GOLD 4D is the most severe.
Clinical features
Symptoms are chronic and progressive.
- Dyspnoea
- Cough
- Sputum production
Patients with chronic bronchitis usually have productive cough and oedema, while patients with emphysema usually don’t have either but have more pronounced dyspnoea. Chronic bronchitis patients are usually characterised by the “blue bloater” phenotype, while emphysema patients are usually characterised by the “pink puffer” phenotype.
People with COPD may experience acute worsening of their symptoms, called exacerbations, explained later.
Diagnosis and evaluation
Spirometry is required for diagnosis, as COPD is defined as a FEV1/FVC ratio of < 0,70 after administration of a bronchodilator. A baseline spirometry is performed, after which the patient is administered a bronchodilator followed by another spirometry.
The bronchodilator test is performed to distinguish COPD from bronchial asthma. If the FEV1 improves more than 12% after bronchodilator, bronchial asthma is diagnosed.
Differential diagnosis:
- Bronchial asthma
- Lung cancer
- Congenital heart failure
- Tuberculosis
Treatment
The goal of the treatment is to reduce symptoms and to reduce risk of disease progression, exacerbations, and mortality. The medical treatment depends on the GOLD stage.
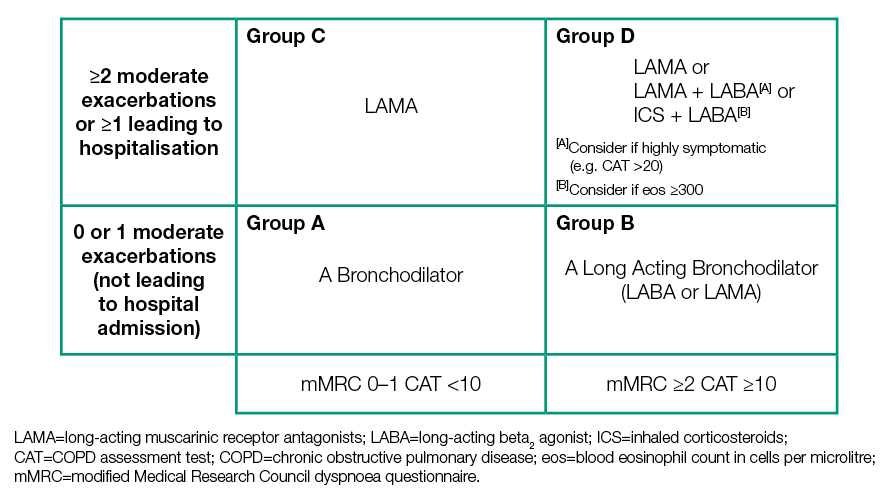
Many drugs are used in the treatment of COPD. This are the most frequently used:
- Short-acting beta agonists (SABA)
- Fenoterol
- Salbutamol
- Long-acting beta agonists (LABA)
- Formoterol
- Salmeterol
- Short-acting muscarinic antagonist (SAMA)
- Ipratropium
- Long-acting muscarinic antagonist (LAMA)
- Tiotropium
- Aclidinium
- Glycopyrronium
- Inhaled corticosteroids (ICS)
- Budesonide
- Fluticasone
Two or three types can be given in the same inhalator.
Non-pharmacologic therapy includes smoking cessation, long-term oxygen therapy, physical activity, pulmonary rehabilitation, and vaccination against influenza and pneumococcus. It’s important to know that the only treatments in COPD that improve the survival in COPD patients are smoking cessation and long-term oxygen therapy. Medical treatment improves symptoms and quality of life, but it does not reduce mortality.
Long-term oxygen therapy (LTOT) refers to the use of oxygen supplementation for more than 15 hours per day in patients with COPD who also have chronic hypoxaemia. This doubles the mean survival time. LTOT is indicated when one of the following apply:
- The patient is stable and the PaO2 < 55 mmHg
- The SaO2 < 89% and signs of cor pulmonale or right heart failure are present, including:
- Pulmonary hypertension
- Peripheral oedema due to heart failure
- Polycytaemia
The contraindications include smoking (explosion risk), poor compliance and adherance to therapy, or if CO2 elevation occurs during LTOT. Nowadays modern O2 concentrators are portable and so the patient is not confined to their homes during LTOT.
Complications
- Both
- Recurrent lower respiratory tract infections
- Chronic bronchitis
- Pulmonary hypertension
- Cor pulmonale
- Emphysema
- Pneumothorax (due to rupture of bullae)
- Weight loss, cachexia
Acute exacerbations of COPD
Introduction and epidemiology
Acute exacerbations of COPD are acute worsenings of symptoms in a patient with COPD. It may be caused by viral respiratory infections, bacterial infections, pollution, or stress.
Exacerbations may vary in intensity from mild to very severe and life-threatening. Rapid assessment of the severity is important.
Clinical features
The cardinal symptoms of acute exacerbations are worsening dyspnoea, worsening cough, increased volume and/or purulence of sputum. In severe cases, respiratory failure may occur. If respiratory failure occurs, or if symptoms are severe, or if the patient has serous comorbidities, or if out-patient treatment has failed to improve symptoms, hospitalization is needed.
Diagnosis and evaluation
The diagnosis is based on clinical symptoms. If there are severe symptoms, ABG is used to assess the level of severity.
Treatment
In mild cases, only an increased dose of an inhaled bronchodilator is necessary, sometimes with the addition of an oral glucocorticoid.
If a bacterial infection is suspected, due to infectious signs or purulent or increased volume of sputum, empiric antibiotics can be given.
In cases more severe cases with respiratory failure, O2 supplement or non-invasive ventilation is used. In very severe cases, ICU admission is necessary.