Page created on September 14, 2021. Last updated on April 12, 2022 at 09:44
Introduction
For introduction, epidemiology, etiology, and classification, see the corresponding pathology 2 topic. For clinical features, and diagnosis and evaluation, see the corresponding internal medicine topic (55).
Treatment
Stages I – III are curable, with metastatic gastric cancer usually being incurable. Cancers located only in the mucosa or submucosa (“early” gastric cancer) may be treated endoscopically or with minimally invasive surgery.
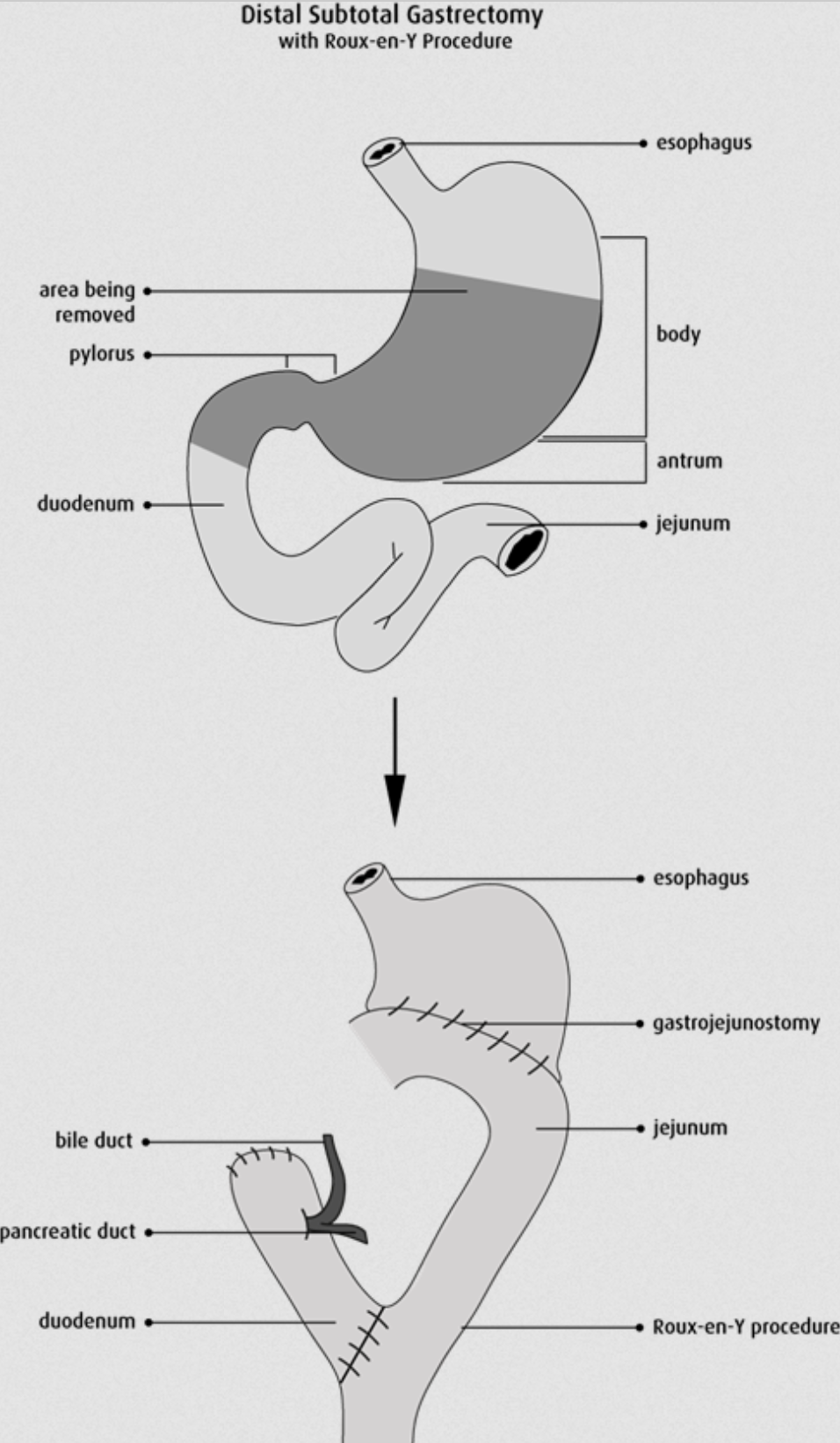
The standard curative surgical treatment for “advanced” gastric cancer patients is radical gastric resection with lymphadenectomy. For intestinal type gastric cancer, distal or subtotal gastric resection is performed. For diffuse type gastric cancer, total gastrectomy is necessary. Afterwards, the GI system must be reconstructed by Roux-en-Y, Billroth I, or Billroth II.
Billroth I refers to the procedure where the distalmost part of the stomach is resected, and an anastomosis is formed between the duodenum and the remaining distalmost part of the stomach in an end-to-end fashion. This can only be performed if the cancer is located distally in the stomach, close to the pylorus. This procedure is rarely performed anymore, and never in the surgical unit of POTE.
Billroth II refers to the procedure where a larger resection of the stomach is performed, and an anastomosis is formed between the side of the duodenum and the side of the remaining stomach in a side-to-side fashion. This procedure allows for a larger resection of the stomach than Billroth I. However, Billroth II allows bile to reflux into the stomach, which causes metaplasia and cancer progression in the remaining stomach or oesophagus. As such, Billroth II is rarely performed anymore, and never in the surgical unit of POTE.
The Roux-en-Y reconstruction surgery is the most frequently performed reconstructive surgery of the proximal GI tract, as it prevents bile reflux. The stomach is separated from the bile-containing duodenum by a strand of jejunum 50 cm long. It is difficult to explain how this works, so I’ll allow this image to do the explaining:
Surgery may be used palliatively as well, in cases where the tumour obstructs passage of foodstuffs, for example. A stent may be placed, the stomach may be resected, or bypass surgery may be employed.
Chemotherapy may be used neoadjuvant for downstaging (to allow for surgery with curative intent), as adjuvant therapy, and as palliative therapy.