Table of Contents
Page created on October 14, 2018. Last updated on December 18, 2024 at 16:56
Obesity
Introduction and definition
Overweight and obesity are states of increased body weight due to adipose tissue accumulation that can contribute to bad health effects. Obesity (and to a lesser extent overweight) is a chronic disease which leads to significant excess morbidity and mortality. It’s also an epidemic that is rising for every year, and is associated with many diseases, including diabetes, hypertension and physical inactivity.
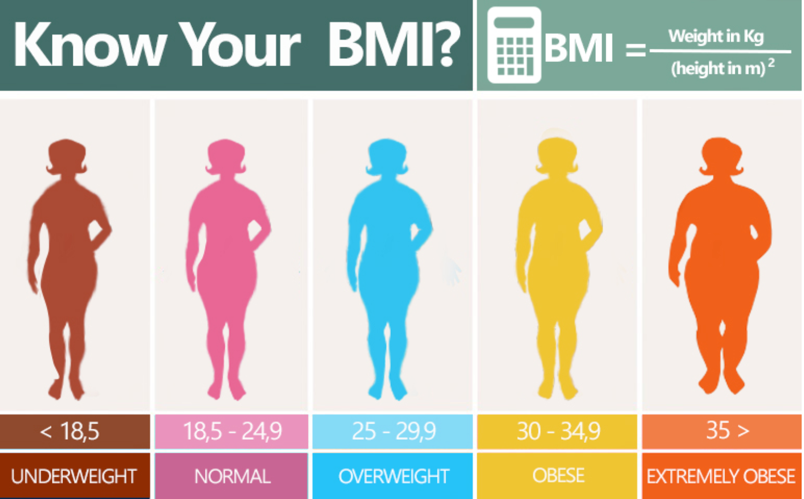
The Body Mass Index (BMI) is used to defined overweight and obesity, although it has its imperfections. It is closely correlated with body fat. However, the BMI will not be the right method to choose if you have a lot of muscle, as the density of muscle tissue is higher than that of fat.
Overweight is defined as a BMI of 25 – 30, while obesity is defined as a BMI > 30. BMI of more than 35 or 40 (depending on the source) is sometimes referred to as morbid obesity.
Etiology
Overweight and obesity is the result of a long-term positive energy balance (more calories in than calories burnt), but the cause of this is multifactorial. Many lifestyle factors, like physical inactivity, poor sleep, and poor diet, are associated with it. However, studies suggest than genetic predisposition accounts for 40 – 70% of the etiology contribution of overweight. Having one overweight parent increases the risk threefold, and having two overweight parents increases the risk tenfold. However, these genetics factors are not due to any single genes but rather many. Research shows that twins who grow up separately with separate foster parents have a body composition more similar to their biological parents than their foster parents.
One theory is the following: The human body evolved to be in activity every day due to unpredictable lives where food was scarce and not readily available. The body is therefore not well adapted to environments where we have too much food and where physical activity is not necessary for survival. In the modern world, there is suddenly a lot of tasty food, but not enough activity.
Important to note that in many countries (like Norway), the average BMI has increased over a period during which the average person ate less and healthier, and worked out more
Types
Obesity can be divided into central and peripheral obesity.
Central obesity, also known as visceral or abdominal obesity, is characterized by fat accumulating in the trunk and in the abdominal cavity around the organs and in the mesentery. Central obesity is more harmful than peripheral obesity. People with central obesity have an increased waist circumference, which is a risk factor for other diseases independent of the BMI itself.
Peripheral obesity is just accumulation in subcutaneous tissue, as in the thighs, breasts and arms.
Complications
Obesity itself is a chronic disease which may lead to a number of other diseases:
- Insulin resistance and type 2 diabetes mellitus
- Cardiovascular disease (ischaemic heart disease, stroke, peripheral vascular disease)
- Hypertension
- Cancer
- Nonalcoholic steatohepatitis
- Cholelithiasis
- GERD
- Osteoarthritis
- Gout
- Infections
- Gynaecomastia
- Decreased fertility
- Pregnancy complications
- Psychosocial problems
- Chronic kidney disease
- Hypoventilation syndrome (Pickwick syndrome)
Overnutrition makes the blood glucose level raise, so the insulin production increases to be able to lower the blood glucose. The insulin receptors will open up for glucose intake, making the cells store glucose as fat. This overnutrition makes the adipocytes full of fat and the muscles and liver full of sugar and glycogen, so they can’t handle any more glucose and shut down their insulin receptors. Pancreas try to produce more and more insulin to lower the sugar levels, but it will all result in hyperglycemia and hyperinsulinemia. High insulin levels prevent lipolysis and fat oxidation, but the patient is still hungry and tired. It becomes a viscous circle.
High levels of insulin may increase levels of Insulin-like-growth-factor-1, (IGF-1), which stimulates growth and survival of cancerous cells. This may explain the increased risk for cancer in obesity.
Diabetes mellitus
Introduction and definition
Diabetes mellitus is not a single disease but rather a group of disorders of carbohydrate metabolism characterised by hyperglycemia. It’s problematic because chronic hyperglycemia is associated with many detrimental health defects, including damage of organs, especially the kidneys, eyes, nerves, and blood vessels. Amputations of lower extremities, blindness in adulthood and end-stage renal disease is very often caused by untreated diabetes.
Hyperglycemia is often a result from defects in insulin secretion or insulin action, or both.
Diagnosis
The diagnosis of diabetes mellitus is made when the patient fulfills any of these three criteria:
- A random blood glucose concentration of >11,1 mmol/L and the patient has typical symptoms of diabetes mellitus
- Fasting glucose concentration of >7 mmol/L
- Abnormal oral glucose tolerance rest (OGTT), where the glucose levels are higher than 11,1 mmol/L 2 hours after 75 g of glucose ingestion.
Typical symptoms of diabetes mellitus include polydipsia (increased thirst), polyuria, low energy and weight loss.
You probably don’t need to know these values.
Types
There are many types of diabetes mellitus, but the two major types are type 1 and type 2. This is the complete classification of DM with subgroups:
- Type 1 diabetes mellitus
- Type 1A (autoimmune)
- Type 1B (idiopathic)
- Latent autoimmune diabetes in adults (LADA)
- Type 2 diabetes mellitus
- Other types of diabetes mellitus
- Maturity onset diabetes of the young (MODY)
- Pancreoprivic diabetes (diseases of exocrine pancreas)
- Cystic fibrosis
- Chronic pancreatitis
- Hereditary haemochromatosis (bronze diabetes)
- Endocrinopathies
- Cushing syndrome
- Acromegaly
- Drug-induced diabetes
- Glucocorticoids
- Antipsychotics
- +++
- Gestational diabetes
Type 1 diabetes mellitus
Type 1 diabetes is an autoimmune disease where the body produces antibodies against the endogenous beta cell antigens. This leads to destruction of the β-cells in the pancreatic islets, so no insulin is produced. This type often develops in childhood, and progress with age.
Exogenous insulin is needed for survival.
Type 2 diabetes mellitus
Type 2 is the most common type of diabetes. It is a prototypical complex multifactorial disease where environment and diet play a major role, and genetic factors may also be involved. It’s characterised by an initial peripheral insulin resistance (peripheral tissues don’t respond properly to insulin), which is compensated for by the beta cells increasing the insulin production. Eventually, beta cells dysfunction and die, so they will no longer be able to compensate for the insulin resistance, at which point chronic hyperglycaemia develops and type 2 diabetes has developed.
Amyloidosis of the Langerhans islets is very common in long-standing type 2 diabetes.
Complications of diabetes
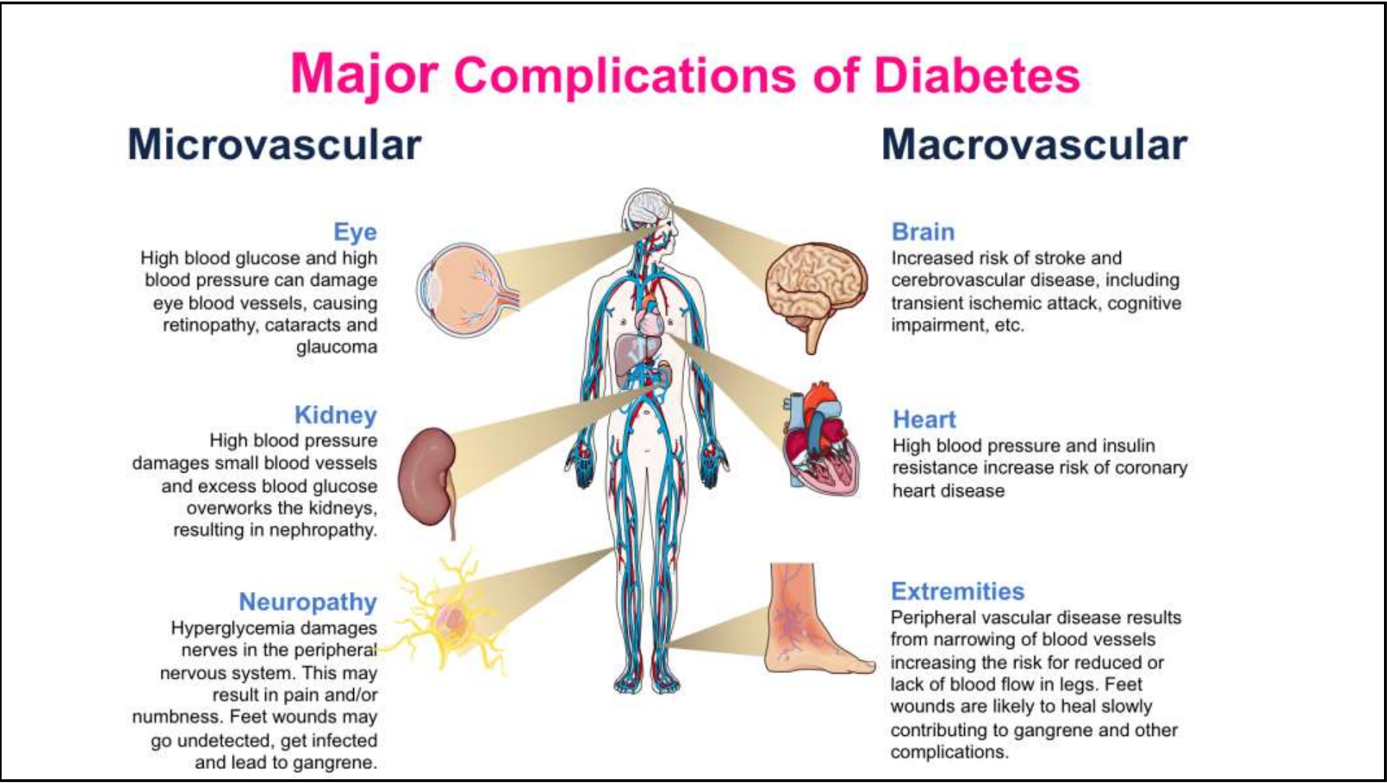
Chronic hyperglycaemia affects both the small and the large vessels, meaning we have both microvascular and macrovascular complications.
- Microvascular complications
- Diabetic retinopathy
- Diabetic neuropathy
- Diabetic nephropathy
- Macrovascular complications
- Coronary artery disease
- Cerebrovascular disease
- Peripheral artery disease
Hyperglycaemia accelerates atherosclerosis which affects the big and medium sized arteries, which increases the risk significantly for atherosclerosis-induced diseases like myocardial infarction and strokes. Peripheral artery disease refers to athersoclerosis of the arteries of the lower extremities, which causes leg pain and gangrene in the worst case.
Management
Different types of diabetes mellitus are treated differently. Type 1 diabetes requires regular insulin injections. Type 2 diabetes is initially treated with medications, but if these aren’t enough to prevent hyperglycaemia, these patients also become insulin-dependent.
What kind of cells are destructed in DM type 1? I think the letter might have fallen out?
Hi!
It seems like the letter beta disappeared! Beta-cells are destructed in DM type 1. Thank you for letting me know 🙂 It is corrected now.