Table of Contents
Page created on October 14, 2018. Last updated on December 18, 2024 at 16:56
Hyperplasia is an increase of the number of cells in an organ or tissue by cell division, resulting in an increase in the mass of the organ.
There are different types of hyperplasia:
Physiologic hyperplasia
There are two types of physiological hyperplasia, hormonal and compensatory.
- Hormonal hyperplasia
- This is the increase of functional capacity of an organ when its needed.
- An example is when a woman is pregante and the glandular epithelium of the breasts starts to proliferate, getting ready for milk production.
- Compensatory hyperplasia
- After damage or partial resection, like after a liver donation. The liver will regenerate itself.
We will discuss them more in detail later in this topic.
Pathologic hyperplasia
A common cause of pathological hyperplasia is the excess of hormones. Estrogen stimulation in the endometrium can lead to abnormal proliferation, and androgens can give a prostatic hyperplasia. This hyperplasia is fortunately under control and there is no mutation in the cell division regulation genes. Also, if the hormone is taken away, the hyperplasia will regress.
Hyperplasia and tumors
Cancer growth is distinct from hyperplasia but can be a “good” starting place to start with cancerous proliferation if hyperplasia is already present. For example, patients with endometrial hyperplasia has a higher chance of endometrial carcinoma.
Cancer growth is not controlled due to mutations of the cell division genes.
Other causes of hyperplasia
During hypoxia, there will be an erythroid hyperplasia in the bone marrow to get enough cells to produce red blood cells.
If there are any antigens present, lymphoid hyperplasia will take place when the lymphocytes multiply as part of the immune response.
Viral infections such as Papillomaviruses can cause skin warts and several mucosal lesions that are composed of hyperplastic epithelium. The virus will make the infected cell produce growth factors, so hyperplasia will be possible.
Mechanisms of hyperplasia
There is either growth-factor dependent proliferation of mature cells or an increased growth of new cells due to stem cell proliferation.
For example: If you have a partial hepatectomy, the growth factors produced in the liver will bind to the surface receptors of the remaining cells and activate signaling pathways to start proliferating. In that way, the part which was taken out can be regenerated.
If this method isn’t possible, like in hepatitis, regeneration will be done by intrahepatic stem cells because the mature cells are compromised.
In which tissues is hyperplasia possible?
We can divide all cells into one of three types: Labile, stable or permanent cells. Labile cells and stable cells can proliferate, while permanent cells cannot.
Labile cells are cells that are continuously in the cell cycle, like epidermis cells and the mucosa of GI-tract that regenerate itself often, so the cells making up these tissues proliferate constantly.
Stable cells are often paused in the G0-phase, but will enter the cell cycle if needed, like hepatocytes in the liver.
Permanent cells never proliferate, like neurons and cardiac myocytes. Brain and heart hyperplasia are therefore impossible.
Now, let’s look at some organ examples
Endometrial hyperplasia
Prolonged estrogen stimuli without switching over to progesterone as it would do normally during ovulation leads to hyperplasia of the endometrium. This estrogen will make the endometrial glands in the stroma proliferate more than normally, and the gland/stroma ratio increases.
The causes of this prolonged estrogen stimuli may be an anovulatory cycle where there is no ovulation because of a persisting follicle. This happens in menopause and puberty.
Other examples of increased estrogen production are obesity or polycystic ovarian disease. In obesity, the big amount of adipose tissue will convert more testosterone into estrogen.
Administration of exogenous estrogens can also cause hyperplasia.
The morphology of endometrial can have two forms; Simple or complex, with or without atypia.
The most common is the simple without atypia. It’s also called a cystic or mild hyperplasia. The glands look like swiss cheese holes, and the gland/stroma ratio is slightly increased. Its fortunately uncommon for this type to transform into cancer, and with estrogen withdrawal it will return to normal by cystic atrophy.
However, simple hyperplasia with atypia is quite rare.
The complex hyperplasia without atypia shows an increase in number and size of glands, and the glands will branch. The level of progression into cancer is still low, compared to complex hyperplasia with atypia, where the morphology overlaps with endometrial carcinoma and the risk for cancer is high. The treatment of complex with atypia is hysterectomy.
A woman with endometrial hyperplasia will experience abnormal bleedings, also called metrorrhagia.
See also this slide.
Prostatic hyperplasia (also called benign prostatic hyperplasia or nodular hyperplasia)
 This condition is extremely common in men over 50 years, and may lead to a narrowing of urethra, making peeing impossible without a catheter in extreme cases. However, only 50 % of the patients have clinically detectable enlargement and symptoms.
This condition is extremely common in men over 50 years, and may lead to a narrowing of urethra, making peeing impossible without a catheter in extreme cases. However, only 50 % of the patients have clinically detectable enlargement and symptoms.
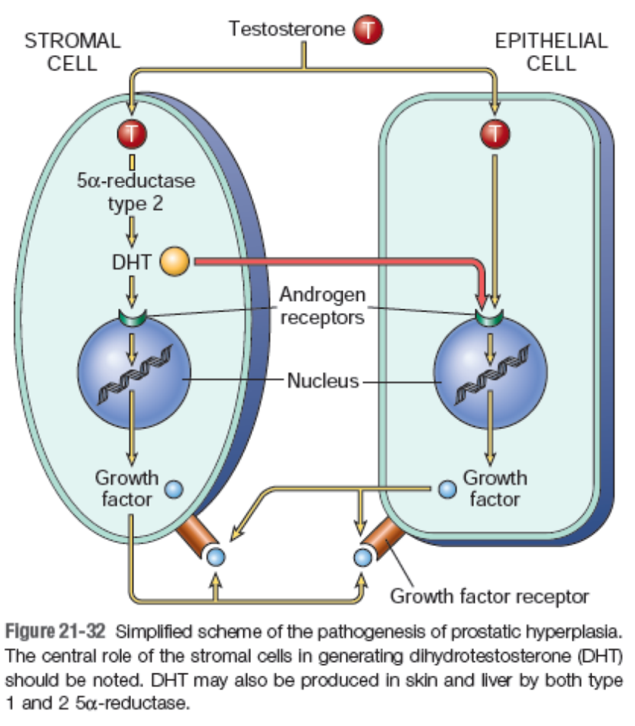
Testosterone gets converted into dihydrotestosterone (DHT) in the stromal cells of the prostate. The DHT will then bind to the androgen receptors of the stromal and epithelial cell nuclei, making the cells produce more growth factor and receptors.
There is no evidence that the periurethral glands actually proliferate, but there is evidence that says the cell death is impaired.
Let’s take a look at the morphology
Macroscopically, we can see that the weight of the prostate is increased. The normal weight of a prostate is disputed among sources, but according to lecture it’s around 25 grams and is the size of a chestnut. Compare this to a hyperplastic prostate, which can weigh over 60 g!
Nodular enlargement of the inner part, also called transition zone, can be seen. The nodules will first be composed entirely of stromal cells, but with further progression there will be epithelial nodules too. This is also called fibromuscular and glandular hyperplasia. The nodules look cystic in appearance with milky fluid.
Microscopically, we see nodularity as well. There are various areas of fibromuscular and glandular proliferation, and the prostatic glands are usually large with basal and secretory layers. The glands also folded and have star-like lumen with eosinophilic secretory material.
The health problems with prostate hyperplasia are many. The urethral obstruction can lead to hypertrophy and dilation of the bladder. Urine retention is also typical, and infections tend to start here and can ascend to the kidneys.
See also this slide and this preparation.
Hey greek, its probably not that important, but in the lecture they said that the normal weight of the prostate is btw 22-25 grams with a size relative to a chestnut.
There is a patho 2 topic about benign prostate hyperplasia, and while writing that I set out to find out what the normal weight and size of the prostate is. Turns out, sources differ wildly. According to lecture it’s 22 – 25 grams and the size of a chestnut. According to UpToDate, it’s 7 – 16 grams and the size of a walnut. This study found the average to be much higher, around 30 – 50 grams.
Anyway, I’ll change the topic to underline what was said in the lecture. This is POTE after all.