Table of Contents
Page created on February 14, 2019. Last updated on May 4, 2022 at 11:50
Written by ms. worldwide, edited by Nikolas.
Congenital malformations
This is basically repetition from embryology, yay…
1. Closure disorders – cleft lip and cleft palate
When the palate fails to close during the embryonic life, and this leads to either cleft lip, cleft palate or both.
These kinds of disorders can result in e.g. feeding problems and speech problems and are operated on while the patient is around 3-12 months old. A palatal obturator is usually used from the birth before surgery, and looks like braces, just for the bone instead of the teeth.

2. Thyroglossal cyst
When the thyroglossal duct from embryonic life persists, a fibrous cyst forms usually on the neck as an irregular neck mass or lump. The cyst develops from left over tissue from the formation of the thyroid gland during development in the uterus.
Recall from embryology that the cysts can occur anywhere of the path of the thyroglossal duct, from the tongue to the suprasternal notch.

Infectious inflammatory disorders of the oral cavity
The infectious inflammations may be caused by either virus, bacteria or fungi. There is a lot to mention, so stray strong!
1. Herpes simplex virus 1 and 2 (HSV 1&2)
Herpes simplex 1 is also known as labial herpes or cold sores and is the most common in the oral region. Herpes simplex 2 mostly occurs on the genitalia, but the incidence of oral HSV2 is increasing since oral sex is getting more and more common. Stop sucking on dirty ding dongs 🤪🍆
Most of us, 70-80 % have antibodies against HSV1, but not everyone get outbreaks. Primary infection is believed to take place already when you’re 2-4 years old. The first attack can be accompanied by fever, sore throat and enlarged lymph nodes. The rash or cold sore disappears by itself, but the virus remains dormant in the trigeminal ganglion. The virus may periodically reactivate and cause new sores. The reactivation can be triggered by:
- Sunlight
- Fever
- Psychological stress
- Menstruation
- Pregnancy
- Upper respiratory tract infections
- Immunosuppression
Primary attacks of HSV1 can in 10-20 % cause an acute gingivostomatitis herpetica, which is basically an onset of multiple vesicles and ulcerations in the whole oral cavity.
Herpes Simplex virus 2 stays dormant in the sacral ganglia.
2. Shingles – Varicella Zoster virus (Herpes virus 3)
The first incidence of the Varicella Zoster virus results in chickenpox. After that, the virus stays dormant in the nerves.
Risk factors for reactivation are old age, poor immune system and getting chickenpox before the age of 18 months. When reactivated, it’s called shingles, and appears as a very painful rash along the dermatomes where the virus was dormant, and usually only on one side. In Norway, we call shingles for “fire from hell” (helvetesild) since it burns pretty bad.
The vaccine reduces the incidence of shingles.

3. Scarlet fever (Scarlatina)
Scarlet fever is a result from group A streptococcus infection which includes symptoms of:
- Sore throat
- Fever
- Headaches
- Swollen lymph nodes
- Strawberry tongue
- Characteristic rash
Long-term scarlet fever can result in kidney disease, rheumatic heart disease and rheumatic arthritis.
4. Corynebacterium diphtheriae
Diphtheria often result in a dense, grey pseudomembrane which covers the tonsils. If its severe enough, it can extend to cover the entire tracheobronchial tree. The bacteria also release diphtheria toxins, which can result in
- Cardiac arrhythmias
- Myocarditis
- Cranial and peripheral nerve palsies

5. Tuberculosis
Apparently, tuberculosis can leave flat ulcers with soft edges in the oral cavity. More about tuberculosis can be studied in the pathology 1 section.
6. Syphilis
If you ever hear the term “lues”, it’s the old name of syphilis. Syphilis, which is very rare nowadays, exists in four stages. In the primary and secondary syphilis, ulcers and lesions can be seen around the mouth and inside the oral cavity.
7. Actinomycosis
This one is also rare and is a granulomatous infection. It is caused by anaerobic, gram positive filamentous bacteria, which are found in the normal flora in the oral cavity, GI-tract and female genital tract. It causes disease first when it gets the opportunity of formation in anoxic environments, like e.g. after dental disease or mandibular osteomyelitis.
It is characterized as lumpy jaw syndrome, with large abscesses located on the head and neck. The abscesses contain sulphur granules.
8. Acute necrotizing ulcerative gingivitis (ANUG)
Caused mostly by anaerobic bacteria, especially fusobacteria and spirochete species. The risk factors are:
- Poor oral hygiene
- Smoking
- Malnutrition
- Psychological stress
- Immunosuppression
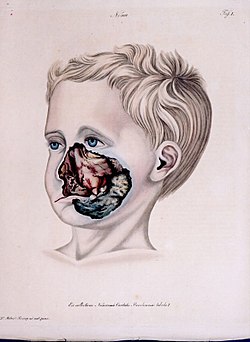
The onset is painful and sudden, and if its severe enough, it can become noma, a gangrenous condition where the tissues of the face undergo necrosis. It’s very painful and deadly. Noma can also occur in the genitals. You can see it illustrated.
 9. Periodontitis
9. Periodontitis
These inflammatory conditions affect the tissue surrounding the teeth, the gums. In the early stage, it’s called gingivitis, where the gums are red, swollen and bleed. If it gets more serious, it’s called periodontitis, where the gums can pull away from the teeth. The teeth can loosen and fall off, and the connection to the bone is lost. It also leads to bad breath.
The major risk factor for this is smoking. The reason for that is that smoking affects the immune system by decreasing wound healing, suppresses the antibody production and reduces neutrophilic phagocytosis.
Periodontitis has also some systemic effects:
- Arteriosclerosis
- Rheumatoid arthritis
- Pregnancy complications
- Alzheimer’s disease
- Chronic conjunctivitis
10. Oral candidiasis/thrush/moniliasis
Oral candidiasis is a fungal infection of the Candida species and affects the mucus membrane of the mouth. This infection is opportunistic.
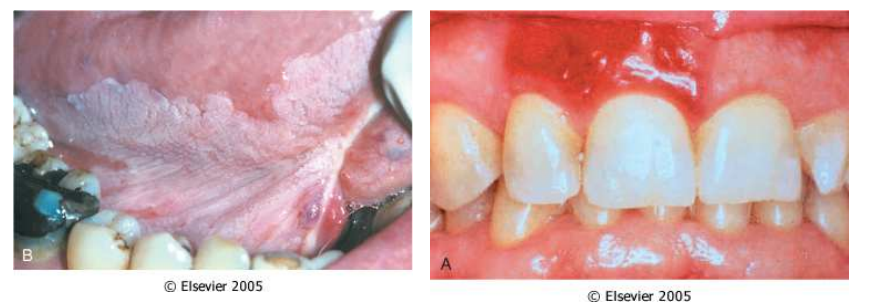
The candidiasis can appear as pseudomembranous, erythematous (atrophic) or hyperplastic (nodular).
Non-infectious inflammatory disorders of the oral cavity
1. Oral lichen planus (OLP)
The most common chronic mucocutaneous disease and affects mostly middle-aged women. It´s mostly a skin disease, but sometimes it only affects the oral cavity with lesions. I can also be found on the glans of penis, vulva and the nails. The etiology is however unknown but is believed to be immune mediated.
The lesions can have different morphology:
- Reticular lesions
- Least painful type
- Erosive/ulcerative lesions
- Most painful type
- Papular lesions
- Plaque-like lesions
- Atrophic
- Bullous
2. Aphthous stomatitis
This is a very common condition, where about 20 % of the general population is affected. It consists of repeated formation of benign and non-contagious mouth ulcers in healthy individuals. The cause for this is a T-cell mediated immune response which is triggered by a variety of factors, like nutrition deficiencies, local trauma, stress, hormonal influences, allergies and genetic predisposition.
3. Pemphigus vulgaris
This is rare chronic blistering skin disease. It is classified as a type II hypersensitivity, where antibodies attack the desmosomes which holds the different layers of the skin attached to each other. This results in big blisters. However, the basal keratinocytes are usually still attached to the basement membrane. This phenomenon is called tombstoning.
The condition affects mostly middle-aged and old patients.
4. Bullous pemphigoid
Also associated with type II hypersensitivity, but the triggering factors are unknown. It mostly affects people over 70 years and is self-limiting.
5. Tumor like lesions – Epulis
Epulis means growth in Greek, and the epulis are usually enlargements of tissue located on the gingiva or the alveoli of the oral cavity. They can be fibromatous, ossifying and acanthomateous.
6. Pyogenic granuloma
This is a lobulated capillary haemangioma and grows rapidly in the gingiva. Looks like a red lump.
Benign tumors
Many of the tumors are associated with the human papilloma virus.
1. Squamous cell papilloma
This is a squamous cell hyperplasia found mostly on the gums and is associated with HPV. If there is multiple papillomas, it’s called papillomatosis.
2. Condyloma acuminatum
This is the same as genital warts but found in the oral cavity and are bigger than the papillomas. It is caused by HPV 6 or 11.
Precancerous and malignant tumors
1. Leukoplakia and erythroplakia
Leukoplakia is an unbrushable white lesion, while the erythoplakias are fiery red. They are associated with increased risk of cancer and have normally no symptoms. The risk factors for leuko- and erythroplakias are smoking, chewing tobacco and excessive alcohol intake.
The risks of progression into invasive squamous cell carcinoma is 3-25 % with leukoplakia, and more than 50 % with erythroplakia. It’s important to distinguish them from benign oral lesions like oral candidiasis.
2. Squamous cell carcinoma
90 % of oral cancers are squamous cell carcinomas. It counts for 3-4 % of all malignant tumors and affects mainly men. The risk factors for squamous cell carcinoma are smoking, alcohol and HPV16. The HPV-associated type affects younger patients that have no history with smoking or drinking alcohol, but they also have a better prognosis than the non-HPV-associated type.
The most frequent locations are lower lip, base of mouth or the both sides of the tongue. It spreads to the lymph nodes in the neck, mediastinum and retropharyngeal lymph nodes, and to the liver, lung and bones with hematogenic spread.
If detected early, the 5-year survival chances are 80 %, but if the tumor is advanced, the chances are only 20 %. So, it’s an aggressive tumor.
The complications from this are
- Cachexia
- Arrosion bleedings
- Aspiration pneumonia
Odontogenic cysts and tumors
A cyst is a pathological cavity lined by epithelium and have accumulation of fluid or gaseous content which is not pus.
1. Dentigerous or follicular cyst
This is a type of odontogenic cysts that are of developmental origin that involve the crown of a unerupted or partially erupted tooth. The cavity of the cyst is lined by epithelial cells derived from the reduced enamel of the unerupted tooth. The pressure from the erupting tooth may obstruct the venous flow, which results in exudate between the reduced enamel epithelial cells and the crown of the tooth.
In other words, this is a cyst which surrounds the crown of a unerupted tooth.

2. Odontogenic keratocyst
Rare, benign but aggressive cyst which affects the posterior mandible. It usually presents in patients around their 30s.
3. Periapical cyst (or radicular cysts or inflammatory cyst)
The most common type of odontogenic cysts and is found in 75 % of cases of cysts in the oral cavity. These cysts surround the apex of the root of a tooth and occur mostly in the anterior region of the maxilla.
Dental caries and trauma to the teeth can lead to pulpal necrosis, which will form the cyst from the epithelial cells’ rests.
Its more common in men and in individuals between 20 and 60 years.
4. Odontogenic tumors
The tumors are derived either from odontogenic epithelium (ameloblast), ectomesenchyme or both.
When from ameloblast, it’s called an ameloblastoma. It doesn’t cause any chondroid or osseous differentiation, but its cystic and infiltrates local tissue. However, its slow growing.
Odontomas are arisen from epithelium but show deposition of enamel and dentin. The tumor can be either hard or soft.
Not only ding dongs, but also 🐱
Nooooooo😭