Table of Contents
Page created on March 16, 2019. Last updated on December 18, 2024 at 16:57
Introduction
This chapter involves mostly disorders of white blood cells. Their number can either be elevated (leukocytosis) or decreased (leukopenia). Leukocytosis itself is nonspecific as it can be a reactive reaction to a primary, often microbial disease, or it can be due to a neoplasm of white blood cells.
Reactive leukocytosis is the increase in white blood cells which is seen in a variety of disorders caused by microbial and nonmicrobial causes. Which specific WBC that has its numbers increased depends on the disease. Here are some examples:
- Neutrophilic leukocytosis
- Acute bacterial infections
- Myocardial infarction
- Eosinophilic leukocytosis (eosinophilia)
- Allergic disorders
- Asthma
- Hay fever
- Parasitic infections
- Certain malignancies
- Allergic disorders
- Basophilic leukocytosis
- Rare. Indicates a malignancy with myeloid proliferation
- Monocytosis
- Chronic infections
- Tuberculosis
- SLE
- IBD
- Chronic infections
- Lymphocytosis
- Chronic infections
- Tuberculosis
- Viral infections
- Hep A
- CMV
- EBV
- Chronic infections
The normal blood cell ranges are:
| Neutrophils | 1.8 – 5.4 x 109/L |
| Eosinophils | 0.0 – 0.5 x 109/L |
| Basophils | 0.0 – 0.08 x 109/L |
| Monocyte |
0.3 – 0.8 x 109/L |
| Lymphocytes | 1.3 – 3.6 x 109/L |
| Red blood cells | 4.5 – 6 x 1012/L |
| Thrombocytes | 140 – 440 x 109/L |
Leukaemia means the presence of lymphoid neoplasias in the circulation. A leukemoid reaction is a strong reactive leukocytosis, with a neutrophil count of above even 30 x 109/L cells! A leukemoid reaction can occur due to severe infection, corticosteroid treatment or stress. Some leukemoid reactions may mimic leukaemia as both cause increased WBC count on a blood test. It’s important to differentiate these two in the clinical practice. The WBCs found in the blood during a leukemoid reaction are usually more mature than those found during leukaemia.
Lymph nodes
Lymphadenopathy is a term that refers to any abnormality of the lymph nodes, like change in size, consistency or number. Lymphadenomegaly describes an enlargement of the lymph nodes, while lymphadenitis refers to its inflammation.
Lymph nodes have two roles. First, they act as filters, as macrophages within the nodes can filtrate the lymph that runs through it. Second, antigen presentation, differentiation and proliferation of B-cells and T-cells occurs in the lymph nodes.
Several properties of the lymph nodes are important in the clinical practice:
- Whether they are painful (tender) or painless (nontender)
- Whether they are soft or firm/hard
- Whether they grow rapidly in size
- Whether they are enlarged
- Whether the abnormal lymph nodes have general or local distribution
- Whether they are movable or fixed
The table below shows how the characteristics of lymph nodes change in different conditions:
| Property | Normal | Acute inflammation | Neoplasm or chronic inflammation |
| Size | < 1 cm | > 1 cm | > 1 cm |
| Consistency |
Soft |
Hard or rubbery | |
| Tender/nontender | Nontender | Tender | Nontender |
| Fixation | Freely movable | Fixed or movable | Fixed to underlying tissue |
Non-specific lymph node changes
Reactive lymphadenitis is a nonspecific response to any immune response against infections or nonmicrobial inflammatory stimuli. The immune cells in the lymph node are activated and start to proliferate. It causes lymphadenomegaly and it can be acute or chronic:
Acute nonspecific lymphadenitis is often a benign response to a localized or systemic infection, and it goes away when the infection is cleared. A localized infection usually causes reactive lymphadenitis in the local lymph nodes while a systemic infection causes generalized reactive lymphadenitis.
Chronic nonspecific lymphadenitis occurs in one of three different patterns, depending on the cause: Follicular hyperplasia, paracortical hyperplasia or sinus histiocytosis.
Follicular hyperplasia is caused by the germinal centre reaction, where B-cells become activated and start to differentiate into immunoglobulin-producing plasma cells and start to proliferate. The follicles contain activated B-cells, some T-cells, antigen-presenting follicular dendritic cells and the tingible body macrophages that phagocytose nuclear debris. Follicular hyperplasia may be due to autoimmune disease or HIV infection.
Paracortical hyperplasia is caused by hyperplasia of the T-cell compartment of the lymph nodes as parafollicular T-cells are activated and start to proliferate. It may occur in lymph nodes near tumors or near inflamed skin (dermatopathic lymphadenopathy) or due to viral infections by e.g. HSV or EBV.
Sinus histiocytosis is caused by hypertrophy of the endothelial cells that line the lymphatic sinusoids and infiltration of histiocytes (macrophages) into the sinusoids. This causes the lymphatic sinusoids to expand. It may occur in anthracosis and Rosai-Dorfman disease.
Specific lymph node changes
Toxoplasma lymphadenitis (or Piringer-Kuchinka lymphadenitis) is the most common clinical form of the disease toxoplasmosis, which is caused by the toxoplasma gondii parasite. This parasite spreads vertically (mother to foetus as part of TORCH) or through the faecal-oral route from cat faeces.
90% of immunocompetent patients develop no symptoms or lymphadenitis when infected with the parasite. The remaining 10% develop mononucleosis-like symptoms with toxoplasma lymphadenitis.
Immunosuppressed patients (transplant patients, AIDS) may develop diffuse toxoplasmosis with toxoplasmic encephalitis.
Intrauterine infection of the foetus increases the risk for spontaneous abortion, intellectual disability and eye abnormalities, among other symptoms.
The histological changes in toxoplasma lymphadenitis can be studied in the slide section. It includes extreme follicular hyperplasia, epithelioid microgranulomas and monocytoid B-cell hyperplasia.
Cat scratch disease is a benign, self-limited lymphadenitis disease caused by the bacterium Bartonella henslae. This bacterium is mainly transmitted by cats via scratching, biting or licking. It causes a swollen, tender regional lymphadenopathy that occurs 2 weeks after the infection and resolves after a few months.
It’s an absceding reticulohistiocytic lymphadenopathy. Histology shows suppurative granulomas, granulomas with central abscess formation, hence the “absceding”. These granulomas have stellate (star-like) shape.
I believe reticulohistiocytic is an old name for the mononuclear phagocyte system, which involves all the tissue macrophages, including histiocytes.
Infectious mononucleosis
Infectious mononucleosis, often called just “mono” or “kissing disease” is an acute self-limited disease of adolescents and young adults that is caused by the Epstein-Barr virus. It’s highly contagious and spreads via bodily secretions, especially saliva. It’s characterized by fever, fatigue, sore throat, generalized lymphadenitis, splenomegaly and lymphocytosis of atypical CD8+ T-cells. It rarely causes symptoms if it occurs during childhood.
As the virus enters the oral cavity will it infect oropharyngeal epithelial cells, from which it spreads to the underlying lymphoid tissue in the tonsils and adenoids where it infects B-cells. The virus lies latent in these cells. Proteins from the virus causes the infected B-cells to undergo polyclonal activation and proliferation, after which they enter the circulation and start to secrete antibodies. These antibodies can be detected in diagnostic tests for mononucleosis, called the Monospot test.
The immune system recognizes that these B-cells are infected and overproliferating. It mounts a T-cell immune response against the cells, which involves virus-specific CD8+ T-cells that kill the EBV-positive B-cells. These CD8+ cells are atypical, and the finding of these atypical cells in the circulation is characteristic for mononucleosis.
The atypical CD8+ cells are large, have abundant cytoplasm and a large nucleus. These cells infiltrate the lymph nodes and spleen, leading to their enlargement. The splenomegaly that occurs in mono is causes the spleen to be especially fragile and prone to rupture after even minor trauma.
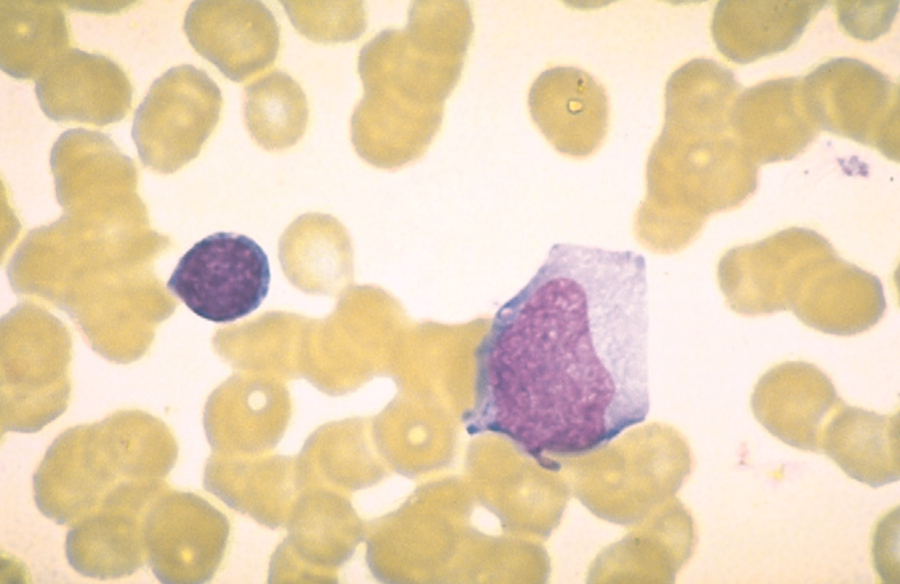
Normal lymphocyte on the left, atypical lymphocyte on the right.
EBV is a potent carcinogenic virus that plays a role in the pathogenesis of many malignancies, including several types of B-cell lymphomas. The importance of a T-cell immunity in mononucleosis can be illustrated as patients lacking T-cell immunity, whether due to immunosuppression, AIDS or genetic defects, have unimpeded EBV-driven B-cell proliferation. This can be fatal if left untreated.
Hey!
Do we have to memorize the ranges of blood cells count?
I would. It’s hard to imagine that they’ll fail you at the patho exam for not knowing, but considering we should know it from physiology it does look quite bad if you don’t even have the slightest idea what the ranges are. Just memorize WBC count (not the individual ones), RBC and platelets. Also, it’s kind of silly to not know the normal WBC range if you’re talking about the elevated WBC count in leukaemia and leukemoid reactions.
A good way of remembering the order of WBC from highest prevalence to lowest prevalence in blood, is to remember = Never Let Monkeys Eat Banana
Neutrophils > Lymphocytes > Monocytes > Eosinophils > Basophils
Maybe it’s helpful 🙂
Throwback to physiology
Hi I think cat scratch disease forms suppurating granuloma without caseous necrosis
I never stated that there was caseous necrosis?
Good afternoon,
what does ”The lymphadenopathy is absceding and reticulohistiocytic. ” means
Thanks a lot
Hey!
Absceding means abscess-forming. I tried really hard to find what reticulohistiocytic means, but I couldn’t find it out. I don’t think it’s that important.