Table of Contents
Page created on February 20, 2019. Last updated on December 18, 2024 at 16:57
Written by ms. worldwide, edited by Nikolas.
Diverticulosis and diverticular disease
Introduction and epidemiology
A colonic diverticulum is a sac-like protrusion of the colonic wall. These diverticula are false diverticula (pseudodiverticula), due to how they involve only the mucosa and submucosa, and not the other layers of the colonic mucous membrane. The presence of many diverticula is called diverticulosis. In some cases, the diverticula may become inflamed. This conditition is called diverticulitis and occurs in approx 10% of people with diverticulosis.
Diverticulosis is usually asymptomatic, but it may cause symptoms like abdominal pain or lower GI tract bleeding. Diverticular disease refers to symptomatic diverticulosis or diverticulitis.
Diverticular disease is mostly a disease of elderly. 60% of people at the age of 60 have diverticulosis. Diverticulosis and diverticular disease is more common in the West, likely due to our eating habits. In the Western world, diverticulosis predominantly affects the left colon, while in Asia, it predominantly affects the right colon.
Etiology and pathomechanism
Colonic diverticula develop under conditions of high intraluminal pressure in the sigmoid colon, and since the colon has the muscle layer gathered at some places as teniae coli, this increased pressure may result in diverticula in these weaknesses where the muscle isn’t present. Exaggerated peristaltic contractions due to diet low in fibre may lead to high luminal pressure. In the western countries, as many as half of the population over 60 years may have this, while the prevalence in Japan and developing countries is much lower. This difference is due to the reduced fibre intake in the well-developed countries.
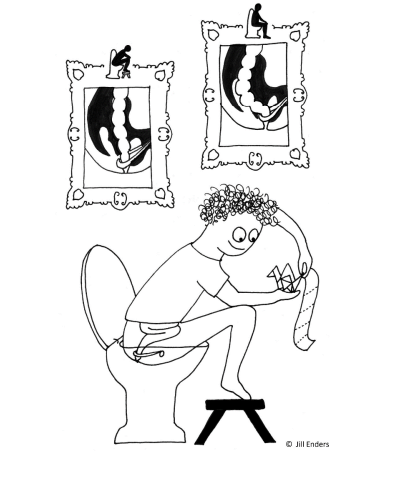
To avoid the development of diverticulosis, its recommended to eat dietary fibre (fresh fruits and vegetables, pasta etc.) and to change the way of sittin’ on the toilet (see the figure below).
The vessels of the diverticula become stretched and therefore weakened, which predisposes to the bleeding which presents are diverticular bleeding.
Diverticulitis occurs due to micro- or macroscopic perforation of a diverticulum, due to erosion of the diverticular wall by increased pressure and food particles. The perforation is usually contained by pericolic fat and mesentery, causing only a simple localised inflammation (simple diverticulitis). However, in some cases, a localised abscess, obstruction, large perforation or fistula may occur (complicated diverticulitis), which may lead to peritonitis.
Polyps of the colon and rectum
Introduction
Colonic polyps are elevated protruding lesions of the colon into the colon lumen. They may be hyperplastic, inflammatory, hamartomatous, or neoplastic. These polyps may cause symptoms or develop into cancer. >90% of colorectal cancers develop from an adenomatous polyp, but only 3 – 5% of adenomatous polyps progress to cancer.
Colon polyps are very common, affecting 30% of adults >50 years.
Classification
- Non-neoplastic polyps
- Inflammatory polyps (pseudopolyps)
- Hyperplastic polyp
- Mucosal polyp
- Neoplastic polyps
- Adenomatous polyps (colorectal adenoma)
- Serrated polyps
- Sessile serrated polyp
- Traditional serrated polyp
- Hamartomatous polyps
Colonic polyps can also be classified according to their macroscopic appearance:
- Pedunculated – have stalk
- Sessile – no stalk
Etiology
Colonic polyps are highly related to the Western, obesogenic lifestyle.
- Diet high in meat and low in vegetables and fruits
- Obesity
- Lack of exercise
- Smoking
- Alcohol
- Hereditary polyposis syndromes
- Familial adenomatous polyposis (FAP) and Gardner syndrome – for adenomatous polyp
- Juvenile polyposis syndrome and Peutz-Jeghers syndrome – for hamartomatous polyp
Inflammatory polyp
Inflammatory polyps are consequences of mucosal ulceration and regeneration, often present in IBD. They don’t have malignant potential.
Hyperplastic polyps
Hyperplastic polyps are consequences of idiopathic mucosal hyperplasia. Mucosal polyps have similar histology as normal mucosa, but often with more goblet cells. Neither have malignant potential.
Adenomatous polyps
Adenomatous polyps, also called colorectal adenomas, are the most important form of polyp, as they have the highest malignant potential, from 5 – 50% depending on subtype, and they’re the most common.
They are characterized by epithelial dysplasia, and these neoplastic mass lesions can range from small pedunculated polyps to large sessile lesions. As many as 50% of the western population over 50 years have these polyps, and since they are known to develop into malignancies, screening should be mandatory when you reach 50 years.
The morphology of the colorectal polyps varies, and they can be:
- Pedunculated, having a stalk with vessels supplying it
- Sessile, having a broad base
- Semisessile, a mix between the two.
More about the morphology of the colorectal polyps can be studied in the slide section.
The following factors indicate a higher malignant risk for adenomatous polyps:
- Multiple
- Large (>2 cm)
- Sessile morphology
- Villous histology
- High grade of dysplasia
Familial adenomatous polyposis (FAP) is an autosomal dominant and caused by the mutation of the adenomatous polyposis coli gene, APC. This disease manifests with hundreds to thousands(!!) polyps in the colon and rectum and start to appear already in the teenage years. They are actually morphologically indistinguishable from colorectal adenomas, so the only way to diagnose a patient with FAP is to count that more than 100 polyps are present.
If a patient with FAP doesn’t get treatment, this patient actually has 100% risk of developing a colorectal adenocarcinoma! And as that isn’t enough, FAP also has different variants like Gardner syndrome and Turcot syndrome.
All patients with FAP must their colon removed to prevent cancer.

Colonoscopy of a patient with FAP. We can see the high number of polyps.
Serrated polyps
Serrated polyps have a characteristic “sawtooth” morphology, which is the etymology of their name. They have moderate malignant potential (5%).
Hamartomatous polyps
Hamartomatous polyps are comprised of normal tissue but with disorganised growth. They may be idiopathic or develop in associated with a syndrome like juvenile polyposis syndrome or Peutz-Jeghers syndrome. Sporadic hamartomatous polyps have no malignant potential, but syndromic hamartomatous polyps do.
Macroscopically, they are pedunculated, round and lobulated. They may also be eroded. Histologically we can see branching and cystically dilated crypts.
Peutz-Jeghers syndrome is a rare autosomal dominant disorder and is characterized by hamartomatous polyps in the whole GI-tract, and mucocutaneous hyperpigmentation. The syndrome also carries higher risks for many malignancies, like breast-, colorectal-, pancreatic-, ovarian-, lung- and stomach cancers. Although the polyps mainly appear in the intestines, they can also occur in the stomach or in the lungs.
Related topics
This is not part of the topic name and will therefore not be asked on the exam.
Aganglionosis
This malformation is the lack of neurons and ganglion cells of the myenteric (Auerbach) and submucous (Meissner) plexus. The most prominent symptom is constipation, followed by vomiting, abdominal pain, diarrhea and slow growth.
This malformation has different names depending on where it affects:
- Hirschsprung’s syndrome is located in the rectum and the sigmoid colon. The major threats for life in new-borns with this are enterocolitis, fluid and electrolyte disturbances, perforation and peritonitis.
Treatment requires surgical resection of the aganglionic part of the colon and anastomosis between the normal parts.
- Long segment aganglionosis includes the rectosigmoid and the proximal colon
- Zuelzer-Wilson syndrome includes the total colon and rectum.
Ischemic colitis
In the colon, ischemia leads to a gangrenous infarction if its severe enough, which can further develop into perforation and sepsis.
90% of all cases occur in patients that are over 60 years old and often together with other morbidities, such as cardiovascular disease. It affects younger people if they had abdominal surgery.
The ischemia can be occlusive or non-occlusive, depending on the cause, like ischemia of the small intestines. The causes can be studied in the previous topic.
Angiodysplasia
Angiodysplasia is a small vascular malformation in the gut. It’s the second most common cause for bleeding from the lower GI-tract after diverticulitis. The incidence increases with age, and affects usually the right colon, but can occur anywhere in the bowels. This manifests as lower GI tract bleeding.
Hei
Under the serrated lesions, isnt it increased epithelial cell turnover, rather than decreased?
Yes, it should be. Fixed now.