Page created on March 24, 2019. Last updated on April 4, 2019 at 11:13
Hyperglycaemia
Defining hyperglycaemia isn’t straightforward, as the plasma glucose value varies depending on stress, recent food intake, circadian cycle and other factors. The diagnosis of hyperglycaemia is necessary for the diagnosis of any type of diabetes mellitus.
Alimentary hyperglycaemia is the hyperglycaemia that occurs after consuming a meal. The degree of which a food causes plasma glucose level to rise depends on that foods glycaemic index. Foods that contain easily absorbable mono-and-disaccharides (like sucrose or fructose) have a high glycaemic index, causing the plasma glucose level to rise rapidly after eating. Foods that contain complex carbohydrates and fibre have a lower glycaemic index and therefore causes less of a plasma glucose level spike after eating. People whose diet contains foods that have lower glycaemic index have lower risk for developing type 2 diabetes, coronary heart disease and obesity.
Relevant blood tests
There are three tools that can be used to diagnose diabetes mellitus. These tools should ideally be used together, especially to confirm diagnosis in uncertain cases. These three tools are:
- Fasting plasma glucose (FPG)
- Oral glucose tolerance test (OGTT)
- HbA1c
The normal and abnormal values of plasma glucose are outlined below:
| Condition | Healthy | Prediabetes | Diabetes mellitus |
| Fasting plasma glucose | 3.5 – 6.0 mmol/L | 6.0 – 7.0 mmol/L (impaired fasting glucose) | > 7.0 mmol/L |
| Oral glucose tolerance test (OGTT) | < 7.8 mmol/L | 7.8 – 11.1 mmol/L (impaired glucose tolerance) | > 11.1 mmol/L |
| HbA1c | < 5.7 % | 5.7 – 6.4 % | > 6.4 % |
The upper normal limit for fasting plasma glucose is 6.0 according to the WHO, but this value is considered too high by many. Other sources, like the American Diabetes Association consider the cut-off value to be 5.6 mmol/L instead. Also, the lecture uses 6 – 8% HbA1c as a normal value, which is crazy and must be a mistake; that corresponds to an average blood glucose level of 7 – 10 mmol/L, which is definitely diabetic.
Fasting plasma glucose: In this scenario “fasting” means going 12 hours without foods or sugary drinks. The normal, healthy range for fasting plasma glucose is below 6.0 mmol/L (below 3.5 is hypoglycaemia). A person who has fasting plasma glucose between 6.0 and 7.0 is considered to have impaired fasting glucose (IFG). A person who has fasting plasma glucose above 7.0 is considered to have manifest diabetes.
The oral glucose tolerance test (OGTT) is an internationally standardized test to test the body’s response to a glucose load. The procedure is like this:
- The patient should eat normally in the days before the test. The patient should not be affected by any illness if possible.
- The patient should fast 12 hours before the test
- At the physician’s office a fasting blood glucose is taken
- The patient is given an oral solution containing 75 g pure glucose that should be consumed within 5 minutes. The patient should be seated for the rest of the procedure.
- Blood may be drawn at 30-minute intervals afterwards, but the most common is to take just one new plasma glucose sample after 2 hours. The plasma glucose level after 2 hours is compared with the table above.
If the 2-hour plasma glucose is below 7.8 mmol/L the patient is healthy. If the value is between 7.8 and 11.1 mmol/L the patient has impaired glucose tolerance (IGT) and is considered pre-diabetic. If the value is above 11.1 mmol/L the patient has diabetes.
Patients with diabetes have reduced insulin response to high blood sugar, either due to low levels of insulin or due to insulin resistance. This reduces insulin response is what causes them to have higher levels of plasma glucose after the glucose load.
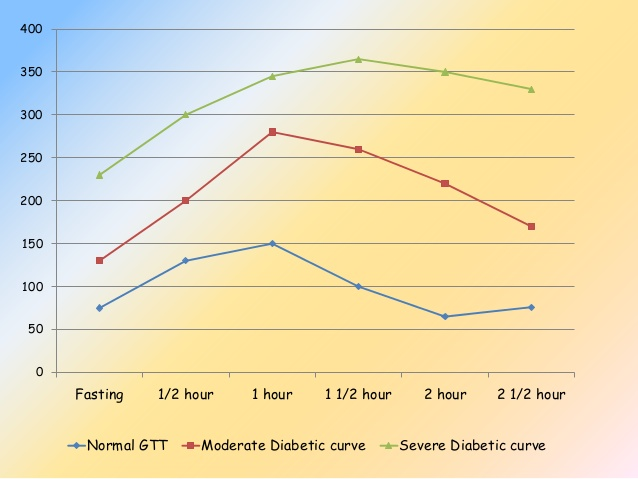
This curve shows how the plasma glucose changes after the OGTT. The units for plasma glucose are different here than what we use. 7.8 mmol/L = 140 mg/dL and 11.1 mmol/L = 200 mg/dL.
The OGTT may be false positive if the level of insulin-antagonist hormones is high, like cortisol or adrenaline. It may also be false positive if the test subject consumes few carbohydrates the day before the test, as this temporarily reduces the insulin-producing capacity of the β-cells.
The test may be false negative is the patient walks or moves during the 2-hour wait, as using the muscles consumes plasma glucose.
HbA1c, also called glycated haemoglobin is a form of haemoglobin that is covalently bound to glucose. It’s formed from non-enzymatic glycation of haemoglobin, which is a normal process that happens even in healthy people. The level of HbA1c corresponds with the average plasma glucose level over three months – this is because RBCs (which contain the glycated haemoglobin) only live for around four months. HbA1c is mainly used to track the blood glucose control of diabetics rather than to diagnose it.
Diagnosis of diabetes mellitus
The diagnosis of diabetes is different depending on whether the patient has symptoms or signs of diabetes or not. Common symptoms include polydipsia, polyuria, blurry vision and weight loss. In patients who show one or more of these symptoms, a single FPG, OGTT or HbA1c test is usually enough to confirm the diagnosis.
It may be necessary to screen persons who don’t show symptoms for diabetes regularly. People who should be screened for diabetes include:
- People who have previously established impaired glucose tolerance (IGT) or impaired fasting glucose (IFG)
- Pregnant women, in weeks 24 – 28
- People above 45 with BMI above 27
- Mothers of very large new-borns
- People with metabolic syndrome
- People whose close relatives have diabetes
These people should perform the OGTT, preferably more than once to confirm the diagnosis.
Other findings may increase suspicion for diabetes as well, like glucosuria, microalbuminuria and ketonuria. The level of C-peptide, which is usually produced in equal amounts as insulin, may indicate which subtype of diabetes the person has. Decreased levels of C-peptide indicate an absolute insulin deficiency and therefore type 1 diabetes. Increased levels of C-peptide indicate hyperinsulinaemia and therefore type 2 diabetes.