Table of Contents
Page created on April 2, 2019. Last updated on May 16, 2019 at 12:01
Introduction
The thyroid gland consists of numerous follicles composed of thyroid follicular cells that surround secreted colloid, a proteinaceous fluid containing large amounts of thyroglobulin, the protein precursor of thyroid hormones. The follicular cells produce thyroglobulin (a large protein) and secretes it into the colloid. The basolateral surface of the follicular cells faces the blood while the apical surface faces the colloid.
Iodine (I) is an important part of the thyroid hormones, and the thyroid very efficiently extracts iodide (I–) from the circulation. After iodide enters the follicular cells it is secreted into the follicle lumen and oxidized into iodine (I), where the iodine binds to tyrosine residues on the thyroglobulin protein. The “iodized” thyroglobulin can then be taken up by the follicular cells, which is processed in lysosomes to release T3 and T4.
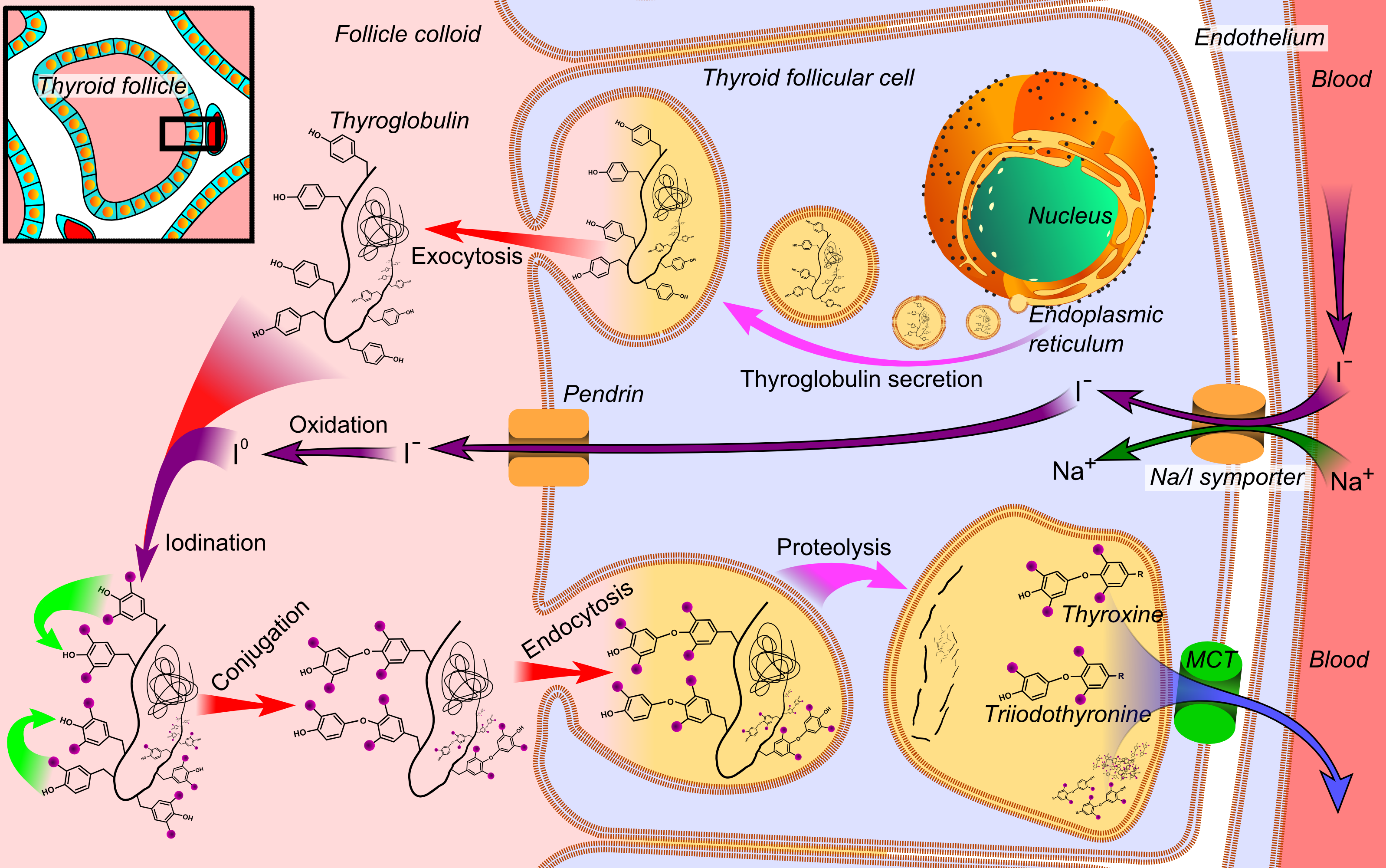
T3 (triiodothyronine) and T4 (thyroxine) are the hormones which are collectively known as “thyroid hormones”. T4 contains 4 iodine atoms while T3 contains 3. T3 is more potent than T4. These hormones act on various tissues throughout the body by acting in intracellular thyroid hormone receptors.
The thyroid hormone receptor binds to DNA and acts as a transcription factor. The effects of thyroid hormone are many:
- Increased BMR
- Increased heat production
- Mobilization and utilization of nutrients and vitamins increases
- Positive heart effects -> increased cardiac output
- Ventilation increases
- GI motility increases
- Growth rate increases in children
- They play an important role in brain development
The regulation of thyroid hormone mostly involves TSH, which again is produced by TRH.
Hyperthyroidism
Thyrotoxicosis is the state where there is an excess of thyroid hormones. Thyrotoxicosis is most frequently the result of hyperthyroidism, but other conditions, like thyroiditis or ingestion of thyroid hormone, may cause thyrotoxicosis without hyperthyroidism.
Hyperthyroidism is the condition where the thyroid function is excessive, which causes thyrotoxicosis. It’s more frequent in women. The most frequent cause is Graves disease, but other causes exist as well, like toxic multinodular goitre and toxic adenoma.
The symptoms of thyrotoxicosis (and hyperthyroidism) are mostly the same regardless of the cause:
- Goitre – enlarged thyroid gland
- Cardiovascular symptoms – T3 increases effects of catecholamines
- Tachycardia
- Palpitations
- Hypertension
- High BMR
- Hyperdefecation – increased frequency of bowel movements
- Osteoporosis
- Myopathy
- Muscle pain
- Muscle weakness
- Heat intolerance
- Moist, warm skin – due to sweating due to increased heat production
- Fine tremor of outstretched fingers
- Restlessness
- Gonadal dysfunction – decreased effect of oestrogen and testosterone
- Amenorrhoea
- Infertility
- Decreased libido
- Erectile dysfunction
Graves disease (sometimes called Basedow disease) is the most common cause of hyperthyroidism. It’s an autoimmune condition where the body produces antibodies that bind to and activate TSH receptors on the thyroid follicular cells, which tricks them into believing that the TSH level is very high.
Risk factors for Graves disease include HLA-DR3, family history of other autoimmune disorders and stress/trauma.
In addition to the symptoms of thyrotoxicosis Graves disease has some characteristic symptoms:
- Graves ophthalmopathy
- Exophthalmos
- Ocular motility disturbances
- Lid retraction
- Dermopathy (pretibial myxoedema)
- Puffy, inflamed skin
- Mostly on legs but can be anywhere
Dermopathy, which was previously called “pretibial myxoedema”, is not the same as myxoedema, which is associated with hypothyroidism. The anti-TSH-receptor antibodies also stimulate fibroblasts in the skin, causing the fibroblasts to produce more glucosaminoglycans like hyaluronic acid. This causes the skin to carry more water. The affected area becomes inflamed, reddish and swollen. Retroorbital dermopathy is what causes Graves ophthalmopathy.
Toxic adenoma is a solitary thyroid nodule that occurs due to a gain-of-function mutation in the TSH-receptor that causes it to be active without stimulation by TSH. This causes focal hyperplasia of thyroid follicular cells, which form a nodule. These cells produce thyroid hormones. The increased level of thyroid hormones produced by this nodule causes negative feedback on the pituitary, which decreases TSH levels. This suppresses the function of the rest of the thyroid, which prevents a more severe thyrotoxicosis.
Thyroid storm
Thyroid storm or thyrotoxic crisis is an acute exacerbation of hyperthyroidism that results in a life-threatening metabolic state. It may be caused by a sudden surge in thyroid hormones or by a sudden surge in catecholamines (as hyperthyroidism increases the effect of catecholamines). Common symptoms include:
- Hyperpyrexia
- Hyperdynamic circulatory failure
- Atrial fibrillation
- Tachycardia with >140 beats per minute
- Severe nausea
- Severe agitation, seizures, potentially coma
Thyrotoxicosis in elderly
The thyroid gland undergoes progressive fibrosis and atrophy with aging, which reduces the functional thyroid volume.
Thyrotoxicosis in elderly tends to present with different symptoms than in younger people. This population usually develops depression, lethargy and weight loss, while symptoms like Hyperdefecation, heat intolerance and tremors may be absent.
Elderly patients with hypertension are more prone to develop angina pectoris or heart failure due to the cardiovascular effects of thyrotoxicosis. Unspecific symptoms like weight loss may be mistaken for an underlying malignancy.
hi greek.doctor
can you please explain how hyperthyroidism leads to hypocalcemia?
it was written in mrt
I can’t find any reliable source supporting that. However, if the hyperthyroidism would be treated surgically, the parathyroid glands would be damaged, which could cause hypocalcaemia. Except from that I don’t think there’s a link between hyperthyroidism and hypocalaemia. In some cases hyperthyroidism may cause hypercalcaemia due to increased bone turnover, though.
thanks, i also found the same thing on the net, the reason i asked this question because my friend had this question on his exam. i could not found any solid evidence about it except in case of surgery.
How will hyperthyroidism cause hypogonadism? I thought that primary hypothyroidism because of increase TRH would increase the prolactin and then cause hypogonadism…
Hyperthyroidism increases the amount of sex hormone binding globulin, which decreases the proportion of free sex steroids in the plasma, mimicking hypogonadism.
sir, will you be continuing writing these amazing notes?
Yes I will, starting tomorrow. Thank you though!
good job buddy
thanks, buddy