via GIPHY
The oral state exam. The last ever exam at medical school.
It’s not known to be difficult; in fact, it’s known to be more of a formality. Virtually no one fail, and people get good grades despite being unable to answer many of their questions.
Even knowing this, the days before the exams were tough. I wasn’t afraid that I wouldn’t pass, but I was still very stressed. I can’t recall the last time I actually couldn’t eat for days due to stress. But hopefully this was the last time.
How it works
On the day of the written state exam (May 25th for us), all 6th year students receive a schedule for the oral state exam, showing you which day you’ll have the exam on. It’s mostly in alphabetical order, and mine was to be June 1st.
On your designated day of oral state exam, at 7:30 in the morning, a Teams group call begins with officials from the university and all the students who are to have their exams that day. There, the officials randomly draw which department each student is to have their exam at. The students must show up at that department at 8:45, and the exam begins at 9.
At 9 you will get a patient to examine. In some departments, mostly ob/gyn and psych, you’re only to take the patient history and not do any physical examination. Following this, there is a practical part where an examiner asks you questions regarding the case and asks you to show certain examinations. This differs a bit from department to department, as some departments combine this “practical examination” with the theoretical examination which comes next.
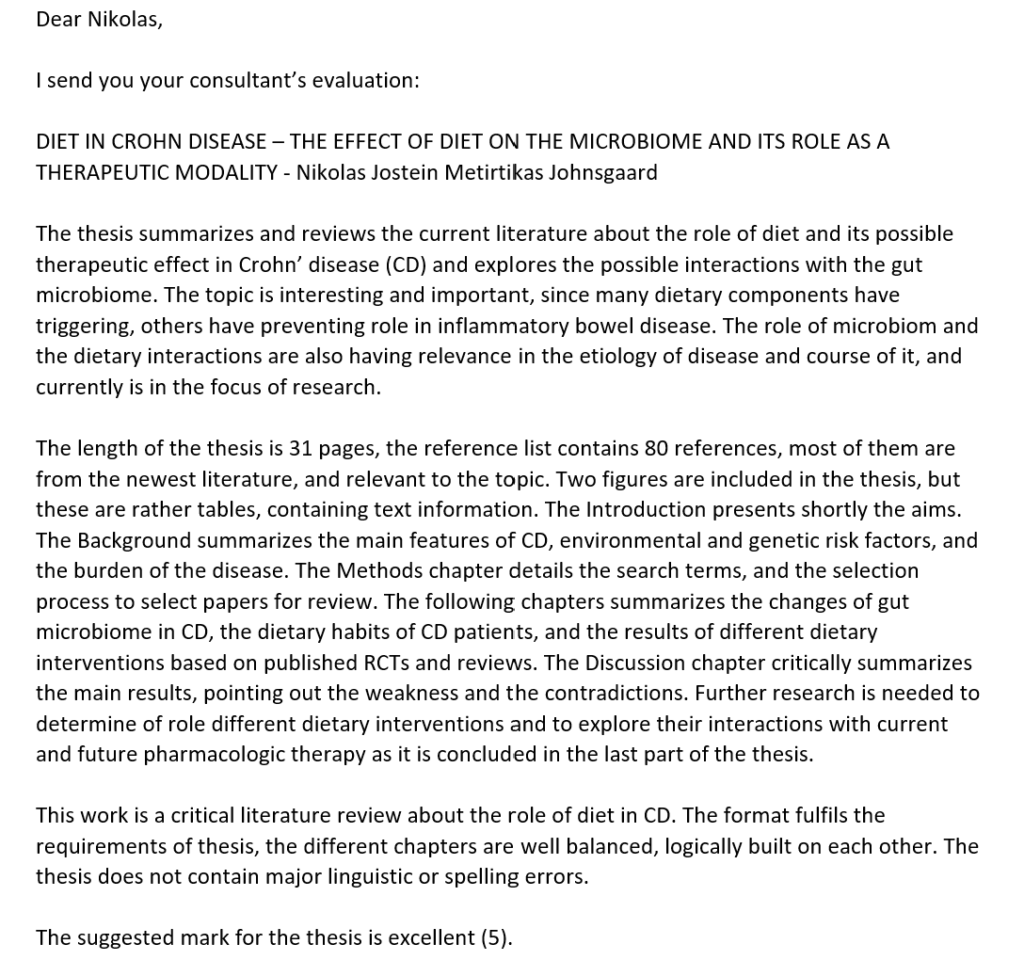
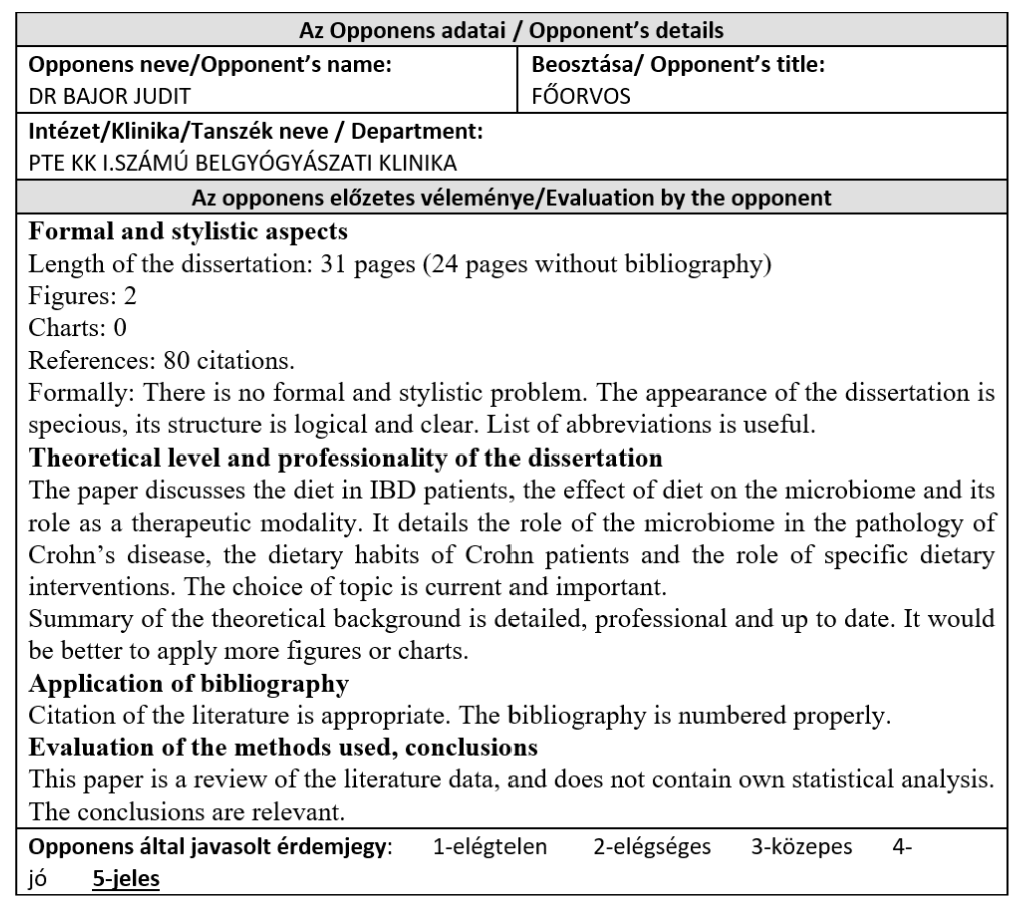
The next is the theoretical examination. In each department 4 – 5 examiners from different departments/specialities form a board which will examine you. Some of these examiners may be from other medical universities in Hungary. They’ll ask you a few questions from their own specialities, and often look at your thesis and ask you a few questions about it as well.
Some departments won’t give you your grade until everyone has finished their theoretical examination that day, while some give it right away. After you get your grade (and a small rite of passage from the examiners), you’re free of the tyranny!
My state exam
The uni officials drew psychiatry department for me. I went there at 8:30. At 9 I get a patient. Many patients at the psychiatry clinic speak English, so students having their exams there usually get an English-speaking patient. Initially, they told me that there were no available English-speaking patients, and that I would have to get one who only speaks Hungarian, but that a resident would help me out, but when I got my patient, they did speak English, so I was glad. We sat down and had a nice chat for some time as I tried to take their medical history.
After I was finished, the resident comes and talks to me about the patient (not to examine me). She shows me the patient’s chart and medication list, explains their findings, and answers my questions about the patient. Then, there was nothing to do but wait for the board.
I was the second to last student to enter the room. The board consisted of prof Tamás Tenyi from psych, prof András Tárnok from paeds, prof Imre Szabó from internal medicine gastroenterology, and prof András Papp from general surgery. They ask for my thesis (but not my ID or skillbook, neither of which I didn’t have to show), and they start skimming it while prof Tenyi asks me to talk about the patient.
My patient had psychotic symptoms, so after I was done presenting the patient, he starts asking questions related to this.
- Tenyi: What is the definition of psychosis?
- Me: It’s when a person loses contact with reality, and their ability of reality testing.
- T: Yes. What are the symptoms of psychosis?
- M: Delusions and hallucinations.
- T: Yes. And?
- I thought those were the only two. I try to think of something, but can’t.
- T: It’s typical in elderly patients.
- M: Delusions of poverty, that they’re being robbed?
- T: Yes but you said delusion already. It’s something different.
- M: Then I don’t know.
- T: What is it called when an elderly patient doesn’t know where they are?
- M: Disorientation.
- T: And is disorientation a symptom of psychosis?
- In my mind, disorientation is unrelated to psychosis
- M: No.
- T: Yes it is. If a patient is in Pécs but thinks they’re in Budapest, they’ve lost contact with reality, so it is psychosis. Right?
- In retrospect I should’ve guessed that the answer was yes based on where this was going.
- M: Yes, makes sense.
- T: Okay. Tell me the eating disorders.
- M: Anorexia nervosa, bulimia nervosa, orthorexia nervosa, and inverse anorexia nervosa.
- T: What are the subtypes of anorexia nervosa?
- M: Binging purging type, and …
- I couldn’t remember the other type
- T: Okay. What are the symptoms of bulimia nervosa?
- M: Binge eating followed by purging, Russel sign on the knuckles, and weight …
- I pause as I suddenly forget whether bulimia patients are low, normal, or high weight
- M: … disturbance
- T: Okay. What is it called when someone is obsessed with healthy eating to the point where they develop malnutrition?
- M: Inverse anorexia nervosa. I mixed them up
- T: No, that’s something else. You said it earlier.
- M: Oh, it’s orthorexia nervosa.
- T: Yes. So what is inverse anorexia nervosa?
- M: It’s when a person like a bodybuilder thinks that they’re small.
- T: Yes. What are the similarities between regular anorexia nervosa and inverse anorexia nervosa?
- M: Both patients cannot see themselves for what they really are. What they see in the mirror is not the truth.
- T: And what is this called?
- M: Body dysmorphia?
- T: No, body image.
- What?
- T: Okay. What is delirium?
- M: Delirium is an acute decline in sensorium and awareness of the environment caused by somatic disease.
- T: Yes. What are the most common causes of delirium?
- M: There can be many causes. Fever, surgery, cancer, infection, metabolic disorders…
- T: Which are the most common metabolic disorders?
- M: Electrolyte disturbances, and-
- T: Which are the electrolyte disturbances most commonly causing delirium?
- I’d never considered this, but the answer is always sodium, right?
- M: Sodium disturbance?
- T: Up or down?
- M: Hyponatraemia.
- T: Yes. What else.
- What else indeed?
- M: Potassium?
- T: No.
- M: Calcium?
- T: No. It’s not an electrolyte.
- M: Oh. Hyperglycaemia?
- T: Can be, but it’s not common.
- I try to think of other metabolic causes, but I’m drawing a blank.
Sometime around this point in time, I realise that there is a lot of tension in the room. Everyone is just staring at me, not smiling, while I mostly look at the floor. A friend of mine had the exam earlier that day with the same board, and he talked about how chill the atmosphere was and how everyone was laughing. When I realised that my exam had a totally different atmosphere, I start to get a bit anxious. Was there tension because I was doing poorly? Or do they not like me?
- Tenyi: Think about an elderly patient who is okay in the morning but in the evening they have delirium.
- That did not help me at all
- T: Think about heart disease, lung disease, …
- Still no clue
- T: … anaemia, …
- M: Hypoxia?
- T: Yes!
- He lets out a small sigh of relief.
- T: Okay, which other metabolic disorders. It’s something you always check in routine labs.
- I try to picture routine labs in my mind
- T: Think about the kidney, liver …
- M: Oh, of course. Liver and kidney failure.
- T: Yes. What is liver failure called?
- M: Cirrhosis?
- T: Yes, but what is the name of the condition when a patient with liver failure develops neurological and psychiatric symptoms?
- M: Oh, hepatic encephalopathy.
- T: Yes. Do you know the name of the tremor?
- M: Flapping tremor
- I made a small flapping motion with my hand as I said it, as if my words weren’t enough to convince them that I knew the answer
- T: Yes. And what is it called for kidney failure?
- I didn’t know what he was after, but I saw an opportunity for a bad joke
- M: Renal encephalopathy?
- They chuckle a bit
- T: No, it’s uraemia.
- Duh.
I think that was the questions I got from psych. He says that he’s finished, and gives the word to prof. Tárnok. He introduces himself, and says that he finds my thesis very interesting as he’s an expert on IBD.
- Tárnok: Do you know what kind of doctor you want to be?
- Me: I’d like to go into internal medicine, probably nephrology or cardiology.
- T: Not gastroenterology?
- M: No, I find nephrology and cardiology more interesting.
- T: Okay, that’s a shame. And may I ask where you’re from?
- M: I’m from Norway.
- T: I looked through your thesis, and it looks very interesting. During researching for your thesis, did you come across the IBSEN study?
- I pretend to think for a bit, but I’m pretty sure that’s not familiar to me
- M: No, I haven’t heard of it.
- T: It is a famous study on IBD which was made in Norway. Anyway. Could you tell me some differences between IBD in childhood and adulthood?
- This is something I’d never really considered. The only difference I could think of at the time was something I’d read while researching for my thesis
- M: Well I know that in children total enteral nutrition is used to induce remission in Crohn disease, but this is not used in adults.
- T: Okay, that is true, but what about the clinical features?
- M: I don’t know
- I don’t remember if he gave me the answer or if he just moved on to the next question
- T: Which is worse, IBD onset in childhood or adulthood?
- I don’t know why, but for some reason I felt that the counterintuitive answer was more correct
- M: In adulthood?
- T: No, childhood IBD is worse. The earlier the onset, the worse the disease.
- I clearly remember that everyone paused at this point, and this awkward moment was perfect to fuel my already high anxiety
- T: Can you tell me a bit about the treatment of Crohn disease in childhood?
- Finally, something I feel like I know
- M: In children we can use either total enteral nutrition or steroids to induce remission, and we can use immunosuppressants like azathioprine or biologics like adalimumab and infliximab to maintain remission
- T: Can we use biological drugs to induce remission?
- M: No, they’re used for maintenance of remission.
- T: That’s not true, they can be used for induction as well. Can you please tell me which drugs for induction of remission induce mucosal healing?
- While studying CD I’ve never heard the term mucosal healing, so I had no idea
- M: Steroids?
- T: No, the biological drugs. Steroids treat the clinical disease but do not induce mucosal healing, while biological drugs do both. Could you explain to me what step up and top down therapy is?
- M: Step up is when you begin with the least intensive treatment and gradually increase it, while top down is the opposite.
- T: Yes, and which do you use in Norway?
- M: Uhm.. I don’t know.
- T: Okay, do you know who decides whether the patient gets step up or top down therapy?
- M: The treating physician?
- T: No, it’s actually the economists. Top down is more effective but is also more expensive, as biological therapy is more expensive. But, it may pay off in the long run due to better outcomes, so these economists must decide whether the initial increased price is compensated by better outcomes in the long run.
- I don’t recall his answer exactly, but it was something like this. Definitely was an unexpected question, at least.
I think he had more questions, but I can’t recall them anymore. Eventually he gives the word to prof. Szabó.
- Szabó: We’ve been talking about IBD so far, which can increase the risk for colorectal cancer. Can you give me some hereditary syndromes which increase the risk for colorectal cancer?
- Me: Gardner syndrome and familial adenomatous polyposis.
- Sz: Yes, and there is one more.
- I try to think, but I can’t recall
- Sz: It’s a non-polyposis syndrome
- I didn’t realise how big of a hint this actually was when he said it
- Sz: It’s hereditary non-polyposis colorectal cancer. Do you know the gene which is mutated in this syndrome?
- I don’t recall, but I do remember some genes involved in CRC.
- M: APC?
- Sz: No.
- M: P53?
- Sz: No.
- Well, those were the ones I could think of initially. But after thinking a bit, I recall something else which is worth guessing
- M: Microsatellite instability?
- Sz: *visibly surprised* Yes, MLH1 or MSH2, for example.
He gives the word to the final member of the board, prof. Papp.
- Papp: I only have one question for you. Could you tell me the differences in surgical treatment for Crohn’s disease and ulcerative colitis?
- Me: So in UC, surgery can be curative, as it only affects the large bowel, and one can remove all of it, but in CD, surgery can never be curative, as the disease will always recur in the areas next to the excised lesion.
- P: Well yes, that’s true, but what I was thinking of was that in CD you only remove the diseased segment of the bowel, while in UC you remove the healthy part as well.
And that was the last question. Before I leave, prof. Tárnok asks whether I’m certain that I don’t want to be a gastroenterologist. Before I can answer, prof. Papp says (in a joking, non-malicious way) “no, it’s too difficult for him”, after which everyone laughed a bit. It may sound rude, but I could tell that he didn’t mean it in a rude way. The fact that everyone laughed made me feel a bit better.
I think I was in for 20 – 25 minutes. In most cases, no one gets their grade until everyone has had their theoretical part, and that was the case for my group as well. Luckily, I was the second to last student, so I only had to wait for one student to finish to get to know my grade.
I felt pretty shit before the exam, but I actually felt even more shit after it. I knew that they don’t fail anyone, but I felt like I answered wrongly on almost every question they had, and I had an unshakeable feeling that I’d failed.
After the last student finishes, they call all the students back into the room where we had the exam. Prof. Tenyi opens with a small “rite of passage” where he says that from this day on, we’re no longer students, but that the medical profession requires regular studying to stay up to date, etc etc. This made me feel pretty secure that I’d passed, but he follows it up with “however, the performances have not been equal” or something like that. He starts by reading the grades of everyone in the order they had the exam.
As soon as they say my name and “five”, I immediately burst into tears, in front of everyone. Like, proper ugly crying. The relief was immeasurable. Luckily I was the second to last student, so I only cried while they were reading the result of one more student. As soon as they finish and congratulate everyone, I turn to hug and cry in a friend of mine’s arms who also had the exam that day.
I leave the room, and outside some of my closest and bestest friends are waiting for me with lots of beautiful flowers and bouquets, and so my crying reinforces as the tears are no longer just tears of tiredness and relief, but from being super touched as well. They see me ugly crying and assume the worst (understandably), but I tell them I got a 5, and they become a bit confused as to why I’m crying so much. While outside, still crying, prof. T´´arnok comes over to shake my hand and congratulate me. Just a bit awkward.
Parting words
A select few graduating students had experiences like me, where they were in for a long time and got asked some difficult questions. The vast majority had really simple, 5 – 10 minute exams with baby questions. But, the most important thing is that, no matter which of these two group you end up belonging to, you’ll pass. The oral state exam is not an exame where anyone fails, but it’s still a source of severe anxiety for many, as it’s the last of the last, and failing it would be devestating. Personally, I was super nervous and lost my appetite for almost a whole week before the exam, and it took some days after the exam for these feelings to disappear. Honestly, by having a terrible oral state exam experience, you’ll leave the university with a proper POTE exam as your last exam experience, which is kind of poetic. Full circle.
In the two weeks since the exam, the graduating students have celebrated, by dancing in a public fountain to the music of a live band (a POTE tradition), by going on a trip to lake Balaton, and by partying a lot. We’ve also rested, for the first time in 6+ years without any school-related worries. Even 2 weeks after finishing, we still have moments of realisation, where we realise that we’re actually actually finished. Our Neptun now shows our student status as “Graduated”. From now on, the adult life starts, and a big chapter of our lives is completed, for good and bad.
I’ll write a post later with what’s next for the website. Even though I’m finished, I still have plans to improve and maintain it, and I’ll definitely not take it down, as many have been worried about.
Congratulations to the graduating class of 2022!