My thesis defence was March 11th. My thesis topic was “Diet in Crohn disease – The effect of diet on the microbiome and its role as a therapeutic modality”. You can read it here. The thesis defence involves defending your thesis against a defence committee consisting of three people, two of which are your designated opponents.
Before the defence
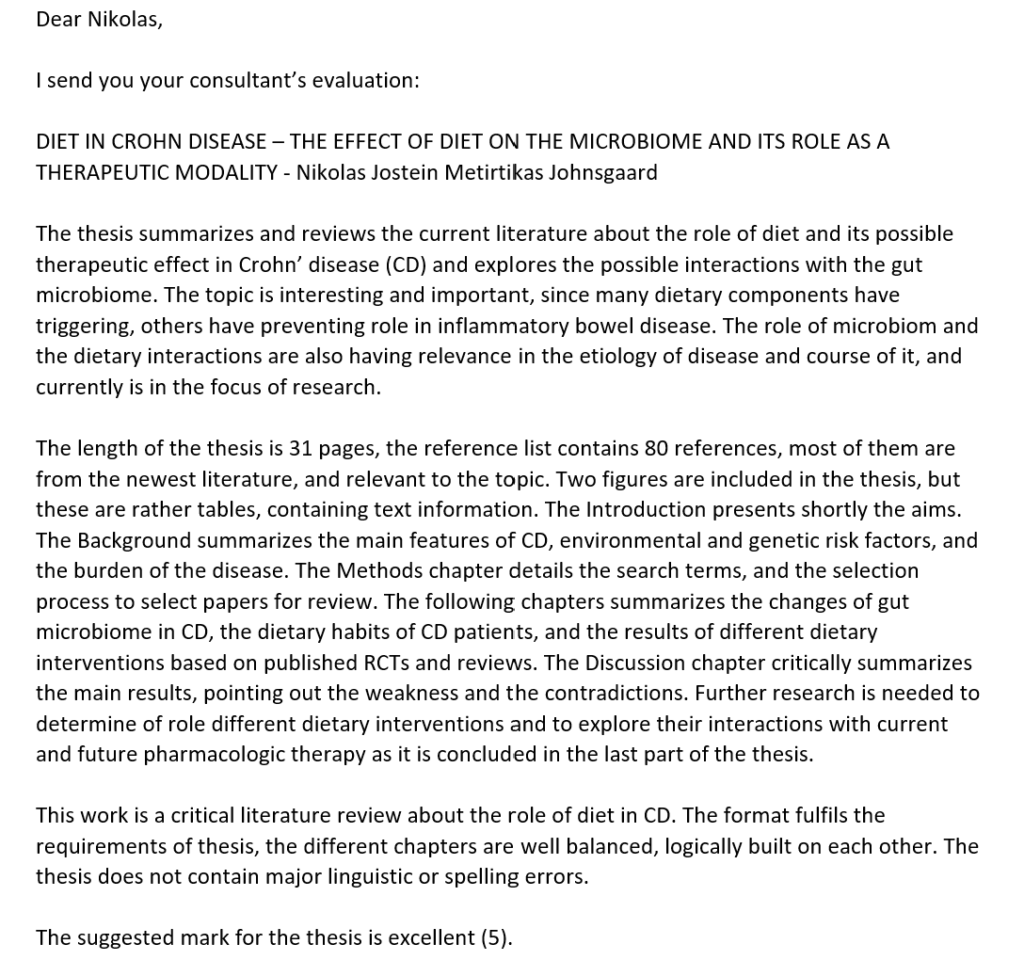
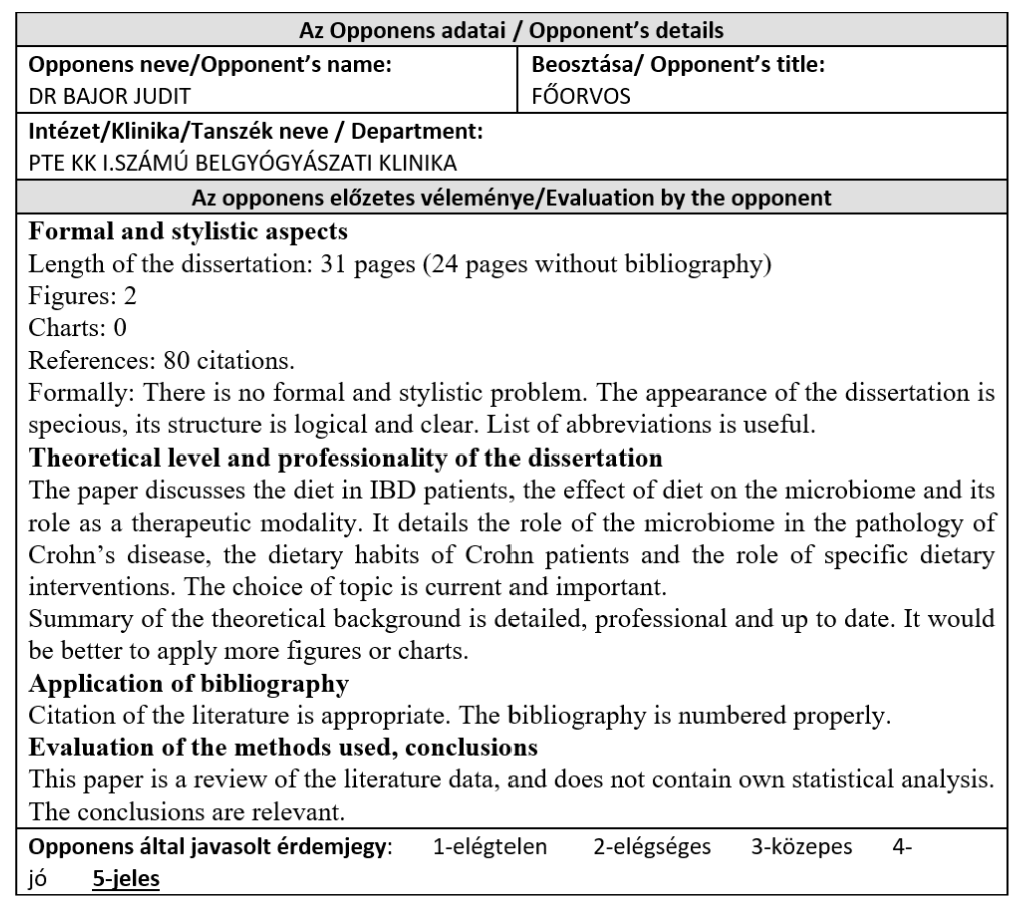
My supervisor was the head of the gastroenterology division of the 1st department of internal medicine, prof. Áron Vincze. Him and dr. Judit Bajor were designated as my two opponents, and as opponents are supposed to do according to the rules, they gave me their separate evaluations of my thesis ahead of the defence.
I was informed of my thesis date by e-mail only 15 days ahead of time, a date they’d chosen without my input. I had already planned a practice in Norway at that date, a practice I had planned 6 months earlier. Plane tickets were already bought. I replied that the date is not appropriate for me, and that we either need to find another date (I had other suggestions which were within the deadline of April 1st) or have it online. The reply was that either of these options would be impossible (even though I know of other students who had it online or were allowed to choose the date themselves). I was also told that the middle of March was the “usual time” during which the 1st department holds its defences, but no one never informed me of this. This means that they were aware of the approximate date of the defence for a long time but decided to inform me only 2 weeks before.
Note that there were no critiques or questions in the opponents’ evaluation. In most cases, students receive questions ahead of time of their defence so they can prepare and answer these questions during the defence. I’d received none.
In most cases, the student is asked to hold a 5 – 10 minute presentation about their thesis during the defence, with or without a PowerPoint presentation. I asked whether I should prepare a pptx, and they replied no, so I assumed I’d have to hold a presentation with no visual help. However, I asked another student who were to have defence with the same department at the same date, and they were told that they shouldn’t have any presentation at all, and that the whole defence should only be reserved for the questions received ahead of time.
So I wasn’t going to hold a presentation, and I hadn’t received any questions. The last days before my defence I was really stressed because I had no idea what I would have to do at the defence. Would I only receive questions for which I couldn’t prepare? Had I received wrong information and would have to hold an impromptu presentation?
Brief summary of my thesis
The gist of it is that there likely exist some possibilities for dietary treatment of Crohn disease, as evidenced mostly by 2 things: Firstly, the well-known efficacy of exclusive enteric nutrition (EEN), the practice of inducing remission in Crohn disease by putting the patient on a nutrition drink-only diet for 6+ weeks, and secondly, the fact that temporarily diverting the faecal stream by using a temporary stoma causes lesions distal to the diversion to heal, and the lesions only recur when the stoma is reversed, which indicates that components in the faeces are important in the development of these lesions. There are a few small studies with special diets for Crohn disease which show some promise, and these diets generally exclude certain food groups (gluten, milk protein, lactose, alcohol) as well as other modifications, but larger studies are needed. As of yet, there is not much evidence to recommend any specific dietary changes in Crohn disease.
The day of the defence
The time of my defence were to be 13:20, so I showed up at approximately 13:00. It turns out that the student who were supposed to start at 13:00 hadn’t started their defence yet, because a member of the defence committee was late, so the whole ordeal was already delayed. While waiting, one member of the defence committee for my defence shows up and waits with us. We have a nice chat, and he tells me that neither of my opponents are present today, so their places on the committee has been replaced by two other doctors. However, according to him, on a defence committee only the opponents have actually read through the thesis, but since both of my opponents were absent that day, none of the members of my defence committee had read through my thesis (although in retrospect I believe one of the members might have read through it on his own initiative, but it’s impossible to know for sure).
He also tells me that I should begin the defence by summarising my thesis in 10 sentences, “of which the first four should be especially good”, and that they’d just ask a few questions and that would be that. I’m glad he told me that, so I at least had a few minutes to mentally prepare some sentences before going in. Eventually, after some delay, it’s my turn.
The defence
They invite me into the library, and ask me to take a seat at the table in front of the three committee members. They are, in no particular order: prof. József Zsimmer, prof. László Czopf, and prof. Imre Szabó. They begin by asking me to briefly summarise the topic of my thesis. I intended to make it 10 sentences but I think it ended up lasting 3 – 4 minutes instead. Some of the questions they followed up with which I remember were:
- What are the main suggestions regarding diet in Crohn disease? (For example exclusion of certain dietary factors like gluten, milk protein, alcohol)
- Do you think that there are any differences between the different stages or extents of the disease regarding these factors in the diet? (Most likely the localisation, severity and type of CD could influence the dietary treatment)
- If there is a patient with fistulising disease and no large bowel affection, what would be your suggestion about the diet? (Here I think I answered that they should avoid dietary fibre, but only because I misheard him so I thought he said stricturing disease, in which case dietary fibre avoidance is correct, but I don’t know what he was going for with this question)
- If you advise dietary restriction to a patient, which by evidence decreases the microbiome diversity, which is potentially harmful, what are the possible correlations with Crohn disease? Are there any evidences or is it too early to talk about? (I think I replied that it’s too early to know, and that during my thesis work I only found evidence of short-term changes in microbiome following dietary modifications in Crohn disease)
- If you analyse a Crohn disease patient for other parallell disorders like food allergies or intolerances, would it change the approach? Do you think these restriction diets work in some cases but not in general because of these comorbidities and not necessarily because of the Crohn disease itself? (I think I answered that yes, that could be a possibility)
- Do you have any data on detailed analysis of the microbiome in Crohn disease patients? (Yes I do, there is a section in my thesis about it. Analysis shows that in general CD patients have less microbiological diversity, lower absolute number of microbes, decreased proportion of “good” gut bacteria and increased proportion of “bad” gut bacteria)
- What is the risk factor if you decrease the microbiome diversity in an autoimmune disease like Crohn disease? Because these restriction diets will decrease the diversity. (I replied that I haven’t seen any studies on whether restriction diets affect the microbiome diversity and whether it has any negative effects on the activity of Crohn disease)
- Do you know of any gastrointestinal diseases which can benefit from modifying the microbiome? (I didn’t know what to answer to this. I only replied small bowel bacterial overgrowth, I think)
- If you would investigate the diet in case of Crohn disease, which approach or direction would seem to be the most feasible for you? (I’m not sure I understood his question correctly, but I think I answered that we could use food questionnaires or asking patients to write down what they eat)
- Do Crohn disease patients have different nutrition than healthy people? (Yes, it’s covered by my thesis that CD patients often avoid foods which they feel make their symptoms worse. They often avoid healthy foods and eat unhealthy foods like soda and snacks)
- Do you consider this to be related to the easier absorption of sugar from these foods? (Yes, that could be an explanation, considering the possibility of malabsorption in CD)
The last line of questioning was the most memorable one:
- Committee member: Based on the results of your thesis, what would be your suggestion to a patient with Crohn disease regarding diet?
- Me: Based on what I’ve read, I’d recommend patients to experiment with their diet, so they could for example exclude one food group from their diet, and—
- C: Based on what? Their relief of symptoms?
- M: Relief of symptoms may be one measure, other could be for example changes in blood tests like CRP level—
- C: Based on CRP you would suggest food diet restriction?
- M: No, just—
- C: This is restriction. If you tell the patient to not eat something, it’s restriction. It can be harmful. You would suggest, without evidence, for the patient to do that?
- M: If they’re interested in trying an approach which is not yet evidence-based, then I would suggest them to restrict certain food groups—
- C: Based on what?
- M: Based on the little evidence that is already present, for example the CD-TREAT diet which I mention in the thesis, which avoids alcohol, lactose-containing milk products and gluten, and these patients have shown good results in inducing remission. So this is—
- C: But that’s not true!
- I’m stunned into silence at this point.
- C: Alcohol okay because it’s harmful, in general we should suggest to avoid it. But you would ask your patient to do a restriction diet, which can be harmful because we know that if you decrease microbiome diversity that’s not a good thing, even without evidence. You should be aware about what you suggest. It can be dangerous. You can not restrict diet if it’s harmful, okay? You can suggest a lot of things, but you’re going to be a medical doctor so you should follow the evidence.
The last line of questioning really took me aback. I don’t know of the evidence that restricting certain food groups can be dangerous like he was talking about, and he obviously wasn’t aware of the studies I was talking about. I suppose vegans, vegetarians, coeliac disease, and lactose intolerance patients worldwide are living dangerously.
Following this, the committee leader thanks me for the presentation and “especially for your work”, which he said he thought was very nice and opens a window into a new area of IBD research. That was very nice of him to say.
Then they started discussing the grade. They check my opponents’ evaluations (both 5), and the leader of the committee suggests 5 as well and asks if the others agree. The member who held the last line of questioning replied that he would give “maximum a 4, maybe even a 3”, but luckily for me the other two members suggested 5 and majority rules. In total, the whole defence took approximately 15 minutes.
And that’s all I have to say about that.